Systemic Sclerosis
All patients with scleroderma have certain shared features of the illness which include:
- Progressive scarring of blood vessels beginning in the fingers but with risk of extending to internal organs
- Scarring of tissues outside the blood vessels including skin thickening and lung involvement
- Varying levels of tissue inflammation and evidence of an overactive immune system
The illness is classified in large measure based on the extent and severity of skin thickening. This is usually done by a simple clinical examination technique called the MODIFIED RODNAN SKIN SCORE:
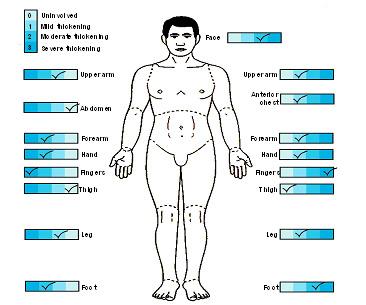
This individual has skin thickening above the elbows and knees and on the chest and would be classified as having systemic sclerosis with diffuse scleroderma.
An individual with skin thickening restricted to the face, forearms, hands and fingers would be said to have systemic sclerosis with limited scleroderma. This clinical picture used to be called the “CREST syndrome”.


Most patients can be accurately classified based on the timing of development of symptoms, their physical findings and by certain laboratory tests. These features are partially summarized below:
Classification of Systemic Sclerosis
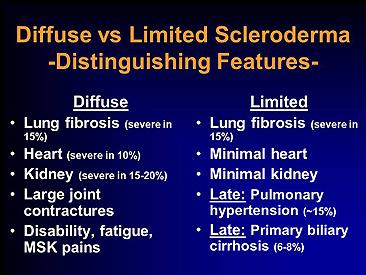
Limited cutaneous scleroderma
- Raynaud phenomenon for years, occasionally decades
- Skin involvement limited to hands, face, feet, and forearms (acral distribution)
- Dilated nailfold capillary loops, usually without capillary drop-out
- A significant (10 to 15 percent) late incidence of pulmonary hypertension, with or without skin calcification, gastrointestinal disease, telangiectasias (CREST syndrome), or interstitial lung disease
- Renal disease rarely occurs
- Anticentromere antibody (ACA) in 70 to 80 percent
Diffuse cutaneous scleroderma
- Raynaud phenomenon followed, within one year, by puffy or hidebound skin changes
- Truncal and acral skin involvement; tendon friction rubs
- Nailfold capillary dilation and capillary drop-out
- Early and significant incidence of renal, interstitial lung, diffuse gastrointestinal,and myocardial disease
- Anti-Scl-70 (30 percent) and anti-RNA polymerase-I, II, or III (12 to 15 percent)antibodies
Scleroderma sine scleroderma
- Presentation with pulmonary fibrosis or renal, cardiac, or gastrointestinal disease
- No skin involvement
- Raynaud phenomenon may be present
- Antinuclear antibodies may be present – anti-Scl-70, ACA, or anti-RNA polymerase-I, II or III
Environmentally induced scleroderma
- Generally diffuse distribution of skin sclerosis and a history of exposure to an environmental agent suspected of causing scleroderma
Overlap syndromes
- Features of systemic sclerosis which coexist with those of another autoimmune rheumatic disease such as systemic lupus erthematosus, rheumatoid arthritis,dermatomyositis, vasculitis, or Sjögren’s syndrome.
Pre-scleroderma
- Raynaud phenomenon
- Nailfold capillary changes and evidence of digital ischemia
- Specific circulating autoantibodies – anti-topoisomerase-l (Scl-70), anti-centromere(ACA), or anti-RNA polymerase-l, II, or III
