Heart Failure: Eating a Healthy Diet
Overview
Why is diet important for heart failure?
Diet is critical in the treatment of heart failure. Limiting sodium is typically recommended to limit fluid build-up. But some other nutrients or substances also play a role as well. Heart failure can become more severe if diet and medicine recommendations for heart failure are not closely followed. Medicine and diet therapy are most effective when used together in the treatment of heart failure.
Taking your medicines and following the diet your doctor has recommended for you will make it easier for you to breathe and help you feel better and be able to do more of your normal daily activities. A registered dietitian can help you make needed dietary changes by providing meal-planning guidelines that are realistic and specifically tailored to your individual needs and preferences.
Ask your doctor if a cardiac rehab program is right for you. Rehab can give you education and support that help you build new healthy habits, such as limiting sodium and eating heart-healthy foods.
Why do you need to limit sodium or fluid?
Sodium
Sodium causes your body to hold on to extra water. This may cause your heart failure symptoms to get worse. Eating too much sodium can even trigger sudden heart failure.
Limiting sodium may help you feel better and prevent sudden heart failure.
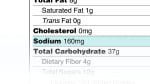
Your doctor will tell you how much sodium you can eat each day. You may need to limit sodium to less than 2,000 mg each day.
Fluid
Fluid intake is not routinely restricted. It may be restricted in advanced cases to maintain your body's electrolyte balance. Closely following your low-sodium diet will help to decrease or eliminate the need for fluid restriction. It is very important that you watch for any signs of fluid gain (swelling or increase in body weight) and report them to your doctor.
Do you need vitamin or mineral supplements?
You can usually get all of your vitamins and minerals by eating a heart-healthy diet that is rich in fruits and vegetables.
Your doctor might recommend a multivitamin/mineral supplement if you are undernourished or cannot completely meet your nutritional needs through food.
If you take a diuretic (water pill) for heart failure, this medicine might change your dietary needs for potassium, magnesium, calcium, and zinc. Ask your doctor if you should take supplements or eat certain foods to get enough of these minerals.
Fish oil (omega-3 fatty acid) supplements have been shown to help some heart failure patients. In some studies, fish oil supplements, taken along with other heart failure medicines, helped people stay out of the hospital and live longer.footnote 1
Talk to your doctor before you take any over-the-counter medicine or supplement. They are used along with medical treatments for heart failure, not instead of treatment.
Potassium
If you take a diuretic, ask your doctor if you need to take a potassium supplement or if you need to watch the amount of potassium in your diet. If you take a loop diuretic or thiazide diuretic, your doctor may suggest that you get extra potassium because these medicines lower your potassium levels. But if you take a potassium-sparing diuretic, you might not need to get extra potassium in your diet.
Magnesium
As with potassium, blood levels of magnesium are typically low with extensive diuretic use. Magnesium plays a role in holding on to potassium in the body. So if you need to replenish potassium, you need to consume enough magnesium also to optimize the body's ability to retain the potassium you are consuming.
Good food sources of magnesium include seeds, nuts, legumes, unmilled cereal grains, and dark green vegetables.
Calcium and zinc
Long-term use of diuretics can also deplete your body of calcium and zinc. Adequate calcium must also be consumed to prevent bone loss, which can occur in people who are not able to be physically active. Good food sources of calcium include milk and milk products, calcium-fortified foods and beverages, broccoli, and kale. Good food sources of zinc include meat, nuts, legumes, fish (especially oysters), poultry, and milk and milk products.
Should you limit alcohol?
Limit alcohol to no more than 1 drink a day, and only if approved by your doctor. Alcohol consumption can make high blood pressure worse and cause further damage to the heart.
What if you need extra calories and nutrients?
In severe heart failure, more calories are often needed because of the increased workload of the heart and lungs. But calorie requirements will vary, based on your current nutritional status.
If you are underweight or malnourished, you will need to increase your intake to obtain sufficient calories and protein to prevent the loss of muscle tissue, maintain or gain weight, and achieve a healthy level of protein (albumin) in the blood.
In people whose activity is very limited (those who are bedridden), it is important to obtain sufficient calories and protein to prevent the development of pressure injuries (bed sores). Increased food intake is often difficult for individuals who have moderate to severe heart failure because of the congestion, poor appetite, shortness of breath, and nausea that are often caused by this condition or by the medicines used to treat it.
The body's increased energy demands along with the obstacles to sufficient intake can often lead to malnutrition in people who have heart failure. The following is a list of suggestions to help you boost your appetite (by reducing fatigue) and to help you increase your calories and protein with as little volume and discomfort as possible.
Tips for increasing your calorie and protein intake
- Eat small, frequent meals (five or six) rather than three large meals each day.
- Eat foods with a soft texture to minimize the amount of chewing you need to do.
- Rest before and after meals.
- Use more of your sodium allowance at your best mealtime of the day to maximize food intake.
- Avoid spicy foods and gas-forming vegetables (such as beans, broccoli, cauliflower, brussels sprouts, cabbage, and onions) if they cause you discomfort (heartburn, feeling of fullness, and gas).
- Drink milk and juices.
- Eat higher-fat meats, milk products, and cheeses.
- Add nonfat dry milk to gravies, sauces, and mashed potatoes (to increase protein intake).
- Add butter or margarine to vegetables, breads, and hot cereals. Use olive oil to saute foods and to top breads.
- Try nuts, peanut butter, and dried fruits for snacks. Eat fruits canned in syrup.
- Talk to your doctor or registered dietitian about including nutrition supplement beverages in your diet if you are malnourished and not able to take in enough food to meet your calorie and protein needs. Those that provide the most calories and protein in each can will provide a lot of nutrition in a smaller volume.
How does heart failure change how your body regulates and uses nutrients?
As heart failure progresses, the heart loses its ability to pump strongly, and blood flow throughout the body decreases. This causes a number of reactions throughout the body. Decreased blood flow to the kidneys hinders their ability to remove excess sodium from the body.
Reduced cardiac output from ineffective pumping stimulates the kidneys to retain fluid. Retained fluid causes congestion in the lungs and difficulty breathing. Excess sodium in the body results in the release of a hormone called aldosterone that causes the body to retain fluid as well. Fluid builds up in the body and causes congestion in the lungs, which makes breathing difficult. Also, fluid may build up in the wall of your intestines, which can make it difficult to absorb nutrients from your food. If your body does not receive the nutrition that it needs, you will lose muscle tissue and your body will not be able to fight off infections.
Credits
Current as of: June 24, 2023
Author: Healthwise Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: June 24, 2023
Author: Healthwise Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.