Polycystic Ovary Syndrome (PCOS)
Condition Basics
What is polycystic ovary syndrome (PCOS)?
Polycystic ovary syndrome (PCOS) is a hormone imbalance that can affect ovulation. It can cause problems with your periods and make it hard to get pregnant. PCOS may also cause other symptoms, such as weight gain, acne, or hair growth on the face or body. If it isn't treated, over time it can lead to serious health problems, such as diabetes and heart disease.
Most of those who have PCOS grow many small cysts on their ovaries. That's why it's called polycystic ovary syndrome.
What does a polycystic ovary look like?
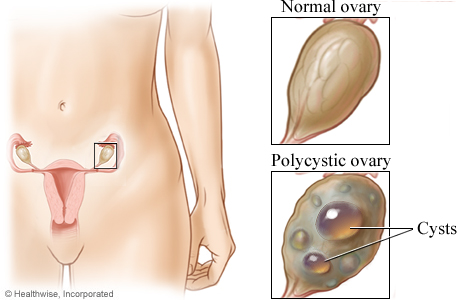
In polycystic ovary syndrome, cysts may form on the ovaries. A cyst is a sac-shaped structure in the body. Cysts usually are filled with fluid.
What causes PCOS?
PCOS is caused by hormones that are out of balance. What causes the imbalance isn't fully understood. But genetics may be a factor. PCOS seems to run in families. Your chance of having it is higher if others in your family have PCOS or have diabetes.
What are the symptoms?
Symptoms of PCOS usually start gradually. They may include acne and oily skin, weight gain and trouble losing weight, extra hair on the face and body, thinning hair on the scalp, irregular periods, problems getting pregnant, and depression. PCOS may be more noticeable after a weight gain.
How is it diagnosed?
To diagnose PCOS, the doctor will ask questions about your symptoms and menstrual cycles. The doctor will also do a physical exam. You'll have some lab tests to check your blood sugar, insulin, and other hormone levels. You may also have an ultrasound to look for cysts on your ovaries.
How is PCOS treated?
Regular exercise, healthy foods, and weight control are the key treatments for PCOS. Your doctor may prescribe birth control pills to reduce symptoms and help regulate your periods, or fertility medicines for problems getting pregnant. Treatment can reduce symptoms and help prevent long-term health problems.
Symptoms
Symptoms of PCOS tend to start gradually. You may have only a few symptoms or a lot of them. Symptoms may include:
- Acne and oily skin.
- Weight gain and trouble losing weight.
- Extra hair on the face and body. You may get thicker, darker facial hair and more hair on your chest, belly, and back.
- Thinning hair on the scalp.
- Irregular periods. Often those with PCOS have fewer than nine periods a year. Some have no periods. Others have heavy bleeding.
- Fertility problems. You may have trouble getting pregnant.
- Depression.
- Insulin resistance and too much insulin. They can cause things like upper body obesity and skin tags.
- Breathing problems while sleeping (obstructive sleep apnea). This is linked to both obesity and insulin resistance.
Hormone changes that lead to PCOS often start in the early teens, after the first menstrual period. Symptoms may be more noticeable after a weight gain.
What Happens
When you have PCOS, your hormones are imbalanced. That can trigger other changes. You may stop ovulating. You may get acne and grow extra facial and body hair, and your chance of getting diabetes may increase. But there are treatments. Treatment can improve symptoms and help prevent serious health problems.
Complications of PCOS
PCOS can affect your reproductive system and how your body handles blood sugar. It can also affect your heart.
Reproductive problems may include:
- Infertility. This happens when the ovaries aren't releasing an egg every month.
- Repeat miscarriages.
- Gestational diabetes during pregnancy.
- Increased blood pressure during pregnancy or delivery, having a larger than normal or smaller than normal baby, or having a premature baby.
- Precancer of the uterine lining (endometrial hyperplasia).
- Uterine (endometrial) cancer.
PCOS can also cause problems with blood sugar. Insulin is a hormone that helps your body's cells get the sugar they need for energy. Sometimes these cells don't fully respond to insulin, which can lead to diabetes.
High insulin levels from PCOS can lead to heart and blood vessel problems. These problems may include:
- Hardening of the arteries (atherosclerosis).
- Coronary artery disease and heart attack.
- High blood pressure.
- High cholesterol.
- Stroke.
Learn more
When to Call a Doctor
Polycystic ovary syndrome (PCOS) causes a wide range of symptoms, so it may be hard to know when to see your doctor. But early diagnosis and treatment will help prevent serious health problems, such as diabetes and heart disease. See your doctor if you have symptoms that suggest PCOS.
Call your doctor now or seek immediate medical care if:
- You have severe vaginal bleeding. You are soaking through your usual pads or tampons every hour for 2 or more hours.
Call your doctor if you have:
- Skipped your period for 3 months or more.
- More vaginal bleeding than usual, or bleeding is more irregular.
- Regular menstrual cycles but you have been trying unsuccessfully to become pregnant for more than 12 months.
- Any symptoms of diabetes, such as increased thirst and frequent urination (especially at night), unexplained increase in appetite, unexplained weight loss, fatigue, blurred vision, or tingling or numbness in your hands or feet.
- Depression or mood swings.
Watchful waiting
Taking a wait-and-see approach (called watchful waiting) is not a good choice if you may have PCOS. Early diagnosis and treatment may help prevent future problems.
Exams and Tests
No single test can show that you have PCOS. To diagnose PCOS, the doctor will:
- Ask questions about your past health, symptoms, and menstrual cycles.
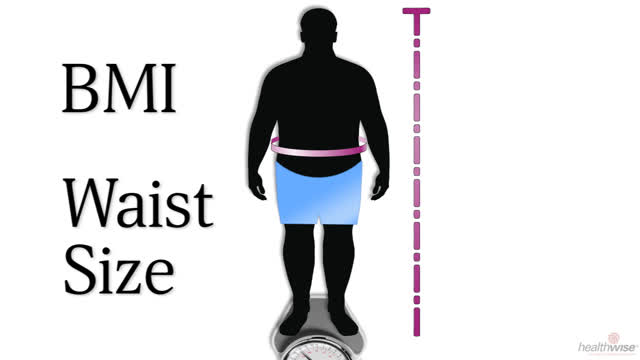
- Do a physical exam to look for signs of PCOS, such as extra body hair and high blood pressure. This may include a pelvic exam. The doctor will also check your height and weight to see if you have a healthy body mass index (BMI).
- Do a number of lab tests to check your blood sugar, insulin, and other hormone levels. Hormone tests can help rule out thyroid or other gland problems that could cause similar symptoms.
You may also have a pelvic ultrasound to look for cysts on your ovaries. Your doctor may be able to tell you that you have PCOS without an ultrasound, but this test will help rule out other problems. Your doctor may do other tests to check for problems caused by PCOS.
Learn more
Watch
Treatment Overview
Regular exercise, healthy foods, and weight control are the key treatments for PCOS. Treatment can reduce unpleasant symptoms and help prevent long-term health problems.
- If you are overweight, weight loss may be all the treatment you need. Even losing 10 lb (4.5 kg) may help balance your hormones.
- Get moderate or vigorous activity often. Walking is a great exercise.
- Eat heart-healthy foods. This includes vegetables, fruits, nuts, beans, and whole grains. Limit foods high in saturated fat.
- If you smoke, think about quitting. If you need help quitting, talk to your doctor about stop-smoking programs and medicines. These can increase your chances of quitting for good.
Your doctor may prescribe birth control pills to reduce symptoms and help regulate your menstrual cycles, or fertility medicines for problems getting pregnant.
It's important to see your doctor for follow-up to make sure that treatment is working.
Self-Care
Home treatment can help you manage the symptoms of PCOS and live a healthy life.
- Eat a balanced diet.
A diet that includes lots of fruits, vegetables, whole grains, and low-fat dairy products supplies your body's nutritional needs, satisfies your hunger, and decreases your cravings. And a healthy diet makes you feel better and have more energy.
You may see a registered dietitian who has special knowledge about diabetes.
- Make physical activity a regular and essential part of your life.
Choose fitness activities that are right for you to help boost your motivation. Walking is one of the best activities. Having a walking or exercise partner that you can count on can also be a great way to stay active.
- Stay at a healthy weight.
This is the weight at which you feel good about yourself, have energy for work and play, and can manage your PCOS symptoms.
Losing weight can be hard, but you can do it. The easiest way to start is by cutting calories and becoming more active.
- If you smoke, think about quitting.
- Care for your skin.
Acne treatment may include nonprescription or prescription medicines that you put on your skin (topical) or take by mouth (oral). You may notice an improvement in your acne after using estrogen-progestin hormone pills.
- Remove or treat unwanted hair.
Excess hair growth (hirsutism) slows when high androgen levels decrease. In the meantime, you can remove or treat unwanted hair with:
- Laser hair removal, in which the hair follicle is destroyed by a laser beam.
- Electrolysis, in which your hair is permanently removed by electric current applied to the hair root.
- Depilatories. These are chemical hair removal products applied to the skin.
- Waxing. This pulls the hair out by the root.
- Shaving.
- Tweezing.
- Bleaching.
Hair removal methods differ in cost and long-term effectiveness. Before trying one, ask your doctor about risks of infection and scarring.
Learn more
Watch
Medicines
As part of treatment for PCOS, medicines can be used to help control reproductive hormone or insulin levels. These medicines can include:
- Combination estrogen and progestin hormones. These are in birth control pills, vaginal rings, and skin patches. These hormones correct irregular or absent menstrual cycles. They may also improve acne problems and reduce unwanted hair growth or loss.
- Progestin. This can help regulate your menstrual period and may help protect against endometrial cancer.
- Androgen-lowering spironolactone. This is often used with estrogen-progestin therapy to reduce acne and unwanted hair growth or loss.
- Metformin. This diabetes medicine is used for controlling insulin, blood sugar levels, and androgen levels.
- Fertility medicines. These include clomiphene and letrozole, and gonadotropin injections (LH and FSH).
Learn more
Infertility Treatments
People who have PCOS and are overweight can try to lose weight. Even a modest weight loss may help improve ovulation. If weight loss doesn't help, then medicines may help.
The medicines letrozole, clomiphene, and metformin may be used to help with ovulation in people who have PCOS. If these medicines don't work, gonadotropins may be tried.
If weight loss and medicines don't work, surgery or IVF may sometimes be an option. A surgery that may be done is ovarian drilling. This involves partly destroying an ovary. It can help with ovulation.
Learn more
Watch
Credits
Current as of: November 27, 2023
Author: Healthwise Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: November 27, 2023
Author: Healthwise Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.