Bile Duct Cancer (Cholangiocarcinoma) Treatment: Treatment - Patient Information [NCI]
This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
What Is Bile Duct Cancer (Cholangiocarcinoma)?
Bile duct cancer is a rare disease in which malignant (cancer) cells form in the bile ducts. Bile duct cancer is also called cholangiocarcinoma.
A network of tubes, called ducts, connects the liver, gallbladder, and small intestine. This network begins in the liver where many small ducts collect bile (a fluid made by the liver to break down fats during digestion). The small ducts come together to form the right and left hepatic ducts, which lead out of the liver. The two ducts join outside the liver and form the common hepatic duct. The cystic duct connects the gallbladder to the common hepatic duct. Bile from the liver passes through the hepatic ducts, common hepatic duct, and cystic duct and is stored in the gallbladder.
When food is being digested, bile stored in the gallbladder is released and passes through the cystic duct to the common bile duct and into the small intestine.
Types of bile duct cancer
There are two types of bile duct cancer:
- Intrahepatic bile duct cancer: This type of cancer forms in the bile ducts inside the liver. Only a small number of bile duct cancers are intrahepatic. Intrahepatic bile duct cancers are also called intrahepatic cholangiocarcinomas.
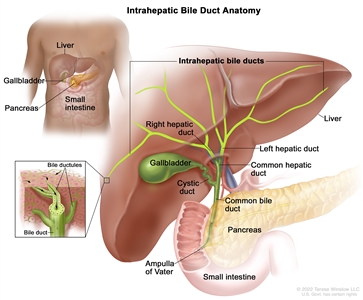
Anatomy of the intrahepatic bile ducts. Intrahepatic bile ducts are a network of small tubes that carry bile inside the liver. The smallest ducts, called ductules, come together to form the right and left hepatic ducts, which lead out of the liver. The two ducts join outside the liver and form the common hepatic duct. The cystic duct from the gallbladder joins the common hepatic duct to form the common bile duct. The common bile duct passes through the pancreas and ends in the small intestine. Bile is made by the liver and stored in the gallbladder. When food is being digested, bile is released from the gallbladder and passes through the pancreas into the small intestine, where it helps digest fats. - Extrahepatic bile duct cancer: This type of cancer forms in the bile ducts outside the liver. The two types of extrahepatic bile duct cancer are perihilar bile duct cancer and distal bile duct cancer:
- Perihilar bile duct cancer: This type of cancer is found in the area where the right and left bile ducts exit the liver and join to form the common hepatic duct. Perihilar bile duct cancer is also called a Klatskin tumor or perihilar cholangiocarcinoma.
- Distal bile duct cancer: This type of cancer is found in the area where the ducts from the liver and gallbladder join to form the common bile duct. The common bile duct passes through the pancreas and ends in the small intestine. Distal bile duct cancer is also called extrahepatic cholangiocarcinoma.
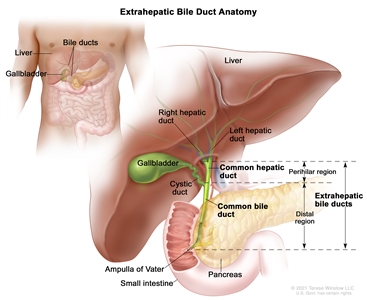
Anatomy of the extrahepatic bile ducts. Extrahepatic bile ducts are small tubes that carry bile from the liver and gallbladder to the small intestine. They are made up of the common hepatic duct (perihilar region) and the common bile duct (distal region). Bile is made in the liver and flows through the common hepatic duct and the cystic duct to the gallbladder, where it is stored. When food is being digested, bile is released from the gallbladder and flows through the common bile duct and pancreas into small intestine.
Signs and symptoms of bile duct cancer
These and other signs and symptoms may be caused by bile duct cancer or by other conditions. Check with your doctor if you have any of the following:
- jaundice (yellowing of the skin or whites of the eyes)
- dark urine
- clay colored stool
- pain in the abdomen
- fever
- itchy skin
- nausea and vomiting
- weight loss for an unknown reason
There are no routine screening tests to check for bile duct cancer before signs and symptoms occur. To learn about tests that are used to diagnose bile duct cancer, see Bile Duct Cancer Diagnosis.
Bile Duct Cancer Causes and Risk Factors
Anything that increases your chance of getting a disease is called a risk factor. There are several risk factors associated with bile duct cancer. Not everyone with one or more of these risk factors will develop the disease, and the disease will develop in some people who don't have any known risk factors. People who think they may be at risk should discuss this with their doctor.
Risk factors for bile duct cancer include the following conditions:
- primary sclerosing cholangitis (a progressive disease in which the bile ducts become blocked by inflammation and scarring)
- chronic ulcerative colitis
- cysts in the bile ducts (cysts block the flow of bile and can cause swollen bile ducts, inflammation, and infection)
- infection with a Chinese liver fluke parasite
There are actions you can take that can help to decrease your risk of getting cancer. To learn more about ways to prevent cancer, see Cancer Prevention Overview.
How is bile duct cancer diagnosed?
Procedures that make pictures of the bile ducts and the nearby area help diagnose bile duct cancer (cholangiocarcinoma) and show how far the cancer has spread. The process used to find out if cancer cells have spread within and around the bile ducts or to distant parts of the body is called staging.
In order to plan treatment, it is important to know if the bile duct cancer can be removed by surgery. Tests and procedures to detect, diagnose, and stage bile duct cancer are usually done at the same time. Every person will not receive all the tests described below.
The following tests and procedures may be used:
- Physical exam and health history: A physical exam of the body will be done to check a person's health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient's health habits and past illnesses and treatments will also be taken.
- Liver function tests: During this procedure a blood sample is checked to measure the amounts of bilirubin and alkaline phosphatase released into the blood by the liver. A higher than normal amount of these substances can be a sign of liver disease that may be caused by bile duct cancer.
- Laboratory tests: These medical tests use samples of tissue, blood, urine, or other substances in the body in order to help diagnose disease, plan and check treatment, or monitor the disease over time.
- Carcinoembryonic antigen (CEA) and CA 19-9 tumor marker test: Tumor markers are released into the blood by organs, tissues, or tumor cells in the body. Increased levels of CEA and CA 19-9 may be a sign of bile duct cancer.
- Ultrasound exam: This procedure uses high-energy sound waves (ultrasound) that are bounced off internal tissues or organs, such as the abdomen, and make echoes. The echoes form a picture of body tissues called a sonogram.
- CT scan (CAT scan): This procedure uses a computer linked to an x-ray machine to make a series of detailed pictures of areas inside the body, such as the abdomen, taken from different angles. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
- Magnetic resonance imaging (MRI): This procedure uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body.
- Magnetic resonance cholangiopancreatography (MRCP): This procedure uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body such as the liver, bile ducts, gallbladder, pancreas, and pancreatic duct.
Different procedures may be used to obtain a sample of tissue and diagnose bile duct cancer. Cells and tissues are removed during a biopsy so they can be viewed under a microscope by a pathologist to check for signs of cancer. The type of procedure used depends on whether the patient is well enough to have surgery.
Types of biopsy procedures include the following:
- Laparoscopy: This surgical procedure is done to look at the organs inside the abdomen, such as the bile ducts and liver, to check for signs of cancer. Small incisions (cuts) are made in the wall of the abdomen and a laparoscope (a thin, lighted tube) is inserted into one of the incisions. Other instruments may be inserted through the same or other incisions to perform procedures such as taking tissue samples to be checked for signs of cancer.
- Percutaneous transhepatic cholangiography (PTC): This procedure is used to x-ray the liver and bile ducts. A thin needle is inserted through the skin below the ribs and into the liver. Dye is injected into the liver or bile ducts and an x-ray is taken. A sample of tissue is removed and checked for signs of cancer. If the bile duct is blocked, a thin, flexible tube called a stent may be left in the liver to drain bile into the small intestine or a collection bag outside the body. This procedure may be used when a patient cannot have surgery.
- Endoscopic retrograde cholangiopancreatography (ERCP): This procedure is used to x-ray the ducts (tubes) that carry bile from the liver to the gallbladder and from the gallbladder to the small intestine. Sometimes bile duct cancer causes these ducts to narrow and block or slow the flow of bile, causing jaundice. An endoscope (thin, tube-like instrument with a light and a lens for viewing) is passed through the mouth and stomach and into the small intestine. Dye is injected through the endoscope into the bile ducts and an x-ray is taken. A sample of tissue is removed and checked for signs of cancer. If the bile duct is blocked, a thin tube may be inserted into the duct to unblock it. This tube (or stent) may be left in place to keep the duct open. This procedure may be used when a patient cannot have surgery.
- Endoscopic ultrasound (EUS): During this procedure an endoscope is inserted into the body, usually through the mouth or rectum. A probe at the end of the endoscope is used to bounce high-energy sound waves (ultrasound) off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram. A sample of tissue is removed and checked for signs of cancer. This procedure is also called endosonography.
What affects bile duct cancer prognosis?
Once bile duct cancer has been diagnosed, the prognosis (chance of recovery) and treatment options depend on the following:
- whether the cancer is in the upper or lower part of the bile duct system
- the stage of the cancer (whether it affects only the bile ducts or has spread to the liver, lymph nodes, or other places in the body)
- whether the cancer has spread to nearby nerves or veins
- whether the cancer can be completely removed by surgery
- whether the patient has other conditions, such as primary sclerosing cholangitis
- whether the level of CA 19-9 is higher than normal
- whether the cancer has just been diagnosed or has recurred (come back)
Treatment options may also depend on the symptoms caused by the cancer. Bile duct cancer is usually found after it has spread and can rarely be completely removed by surgery. Palliative therapy may relieve symptoms and improve the patient's quality of life.
Bile Duct Cancer Stages
This page describes the stages of bile duct cancer (cholangiocarcinoma) for adults. The stage describes the extent of cancer in the body. Knowing the stage helps the doctor plan the best treatment. Bile duct cancer stages are described using the TNM staging system. To learn more about TNM and how cancer stages are described, see Cancer Staging.
To learn about the tests and procedures used to diagnose and stage bile duct cancer, see Bile Duct Cancer Diagnosis.
Intrahepatic bile duct cancer
- Stage 0: In stage 0 intrahepatic bile duct cancer (carcinoma in situ), abnormal cells are found in the innermost layer of tissue lining the intrahepatic bile duct. These abnormal cells are not actually cancer but may become cancer and spread into nearby normal tissue.
- Stage I: Stage I intrahepatic bile duct cancer is divided into stages IA and IB.
- In stage IA, cancer has formed in an intrahepatic bile duct and the tumor is 5 centimeters or smaller.
- In stage IB, cancer has formed in an intrahepatic bile duct and the tumor is larger than 5 centimeters.
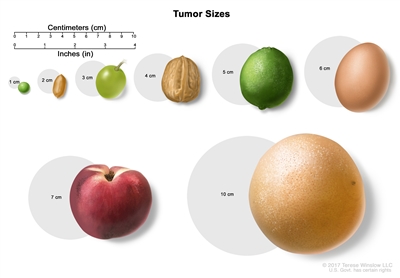
Tumor sizes are often measured in centimeters (cm) or inches. Common food items that can be used to show tumor size in cm include: a pea (1 cm), a peanut (2 cm), a grape (3 cm), a walnut (4 cm), a lime (5 cm or 2 inches), an egg (6 cm), a peach (7 cm), and a grapefruit (10 cm or 4 inches). - Stage II: In stage II intrahepatic bile duct cancer, either of the following is found:
- the tumor has spread through the wall of an intrahepatic bile duct and into a blood vessel; or
- more than one tumor has formed in the intrahepatic bile duct and may have spread into a blood vessel.
- Stage III: Stage III intrahepatic bile duct cancer is divided into stages IIIA and IIIB.
- In stage IIIA, the tumor has spread through the capsule (outer lining) of the liver.
- In stage IIIB, cancer has spread to organs or tissues near the liver, such as the duodenum, colon, stomach, common bile duct, abdominal wall, diaphragm, or the part of the vena cava behind the liver, or the cancer has spread to nearby lymph nodes.
- Stage IV: In stage IV intrahepatic bile duct cancer, cancer has spread to other parts of the body, such as the bone, lungs, distant lymph nodes, or tissue lining the wall of the abdomen and most organs in the abdomen.
Perihilar bile duct cancer
- Stage 0: In stage 0 perihilar bile duct cancer (carcinoma in situ), abnormal cells are found in the innermost layer of tissue lining the perihilar bile duct. These abnormal cells are not actually cancer but may become cancer and spread into nearby normal tissue. Stage 0 is also called high-grade dysplasia.
- Stage I: In stage I perihilar bile duct cancer, cancer has formed in the innermost layer of tissue lining the perihilar bile duct and has spread into the muscle layer or fibrous tissue layer of the perihilar bile duct wall.
- Stage II: In stage II perihilar bile duct cancer, cancer has spread through the wall of the perihilar bile duct to nearby fatty tissue or to liver tissue.
- Stage III: Stage III perihilar bile duct cancer is divided into stages IIIA, IIIB, and IIIC.
- Stage IIIA: Cancer has spread to branches on one side of the hepatic artery or of the portal vein.
- Stage IIIB: Cancer has spread to one or more of the following:
- the main part of the portal vein or its branches on both sides
- the common hepatic artery
- the right hepatic duct and the left branch of the hepatic artery or of the portal vein
- the left hepatic duct and the right branch of the hepatic artery or of the portal vein
- Stage IIIC: Cancer has spread to 1 to 3 nearby lymph nodes.
- Stage IV: Stage IV perihilar bile duct cancer is divided into stages IVA and IVB.
- Stage IVA: Cancer has spread to 4 or more nearby lymph nodes.
- Stage IVB: Cancer has spread to other parts of the body, such as the liver, lung, bone, brain, skin, distant lymph nodes, or tissue lining the wall of the abdomen and most organs in the abdomen.
Distal bile duct cancer
- Stage 0: In stage 0 distal bile duct cancer (carcinoma in situ), abnormal cells are found in the innermost layer of tissue lining the distal bile duct. These abnormal cells are not actually cancer but may become cancer and spread into nearby normal tissue. Stage 0 is also called high-grade dysplasia.
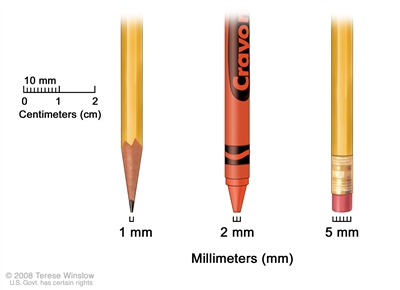
Millimeters (mm). A sharp pencil point is about 1 mm, a new crayon point is about 2 mm, and a new pencil eraser is about 5 mm. - Stage I: In stage I distal bile duct cancer, cancer has formed and spread fewer than 5 millimeters into the wall of the distal bile duct.
- Stage II: Stage II distal bile duct cancer is divided into stages IIA and IIB.
- Stage IIA: Cancer has spread
- fewer than 5 millimeters into the wall of the distal bile duct and has spread to 1 to 3 nearby lymph nodes; or
- 5 to 12 millimeters into the wall of the distal bile duct.
- Stage IIB: Cancer has spread 5 millimeters or more into the wall of the distal bile duct. Cancer may have spread to 1 to 3 nearby lymph nodes.
- Stage IIA: Cancer has spread
- Stage III: Stage III distal bile duct cancer is divided into stages IIIA and IIIB.
- Stage IIIA: Cancer has spread into the wall of the distal bile duct and to 4 or more nearby lymph nodes.
- Stage IIIB: Cancer has spread to the large vessels that carry blood to the organs in the abdomen. Cancer may have spread to 1 or more nearby lymph nodes.
- Stage IV: In stage IV distal bile duct cancer, cancer has spread to other parts of the body, such as the liver, lungs, or tissue lining the wall of the abdomen and most organs in the abdomen.
For bile duct cancer, the following groups are used to plan treatment:
Resectable (localized) bile duct cancer
The cancer is in an area, such as the lower part of the common bile duct or perihilar area, where it can be removed completely by surgery.
Unresectable (including metastatic and recurrent) bile duct cancer
Unresectable cancer cannot be removed completely by surgery. Most patients with bile duct cancer cannot have their cancer completely removed by surgery.
Metastasis is the spread of cancer from the primary site (place where it started) to other places in the body. Metastatic bile duct cancer may have spread to the liver, other parts of the abdominal cavity, or to distant parts of the body. To learn more about metastatic cancer, see Metastatic Cancer: When Cancer Spreads.
Recurrent bile duct cancer is cancer that has come back after treatment. The cancer may come back in the bile ducts, liver, or gallbladder. Less often, it may come back in distant parts of the body. To learn more about recurrent cancer, see Recurrent Cancer: When Cancer Comes Back.
To learn about treatment options, see Bile Duct Cancer Treatment.
Bile Duct Cancer Treatment
This page describes the different types of treatment for bile duct cancer (cholangiocarcinoma). Which of these treatments a patient receives will depend on whether the cancer can be completely removed with surgery (resectable) or not (unresectable). To learn more, see treatment of resectable and treatment of unresectable bile duct cancer.
Types of treatment
Surgery
The following types of surgery are used to treat bile duct cancer:
- Removal of the bile duct: This surgical procedure is done to remove part of the bile duct if the tumor is small and is in the bile duct only. Lymph nodes are removed and tissue from the lymph nodes is viewed under a microscope to see if there is cancer.
- Partial hepatectomy: This is a surgical procedure to remove the part of the liver where cancer is found. The part removed may be a wedge of tissue, an entire lobe, or a larger part of the liver, along with some normal tissue around it.
- Whipple procedure: During this surgical procedure the head of the pancreas, the gallbladder, part of the stomach, part of the small intestine, and the bile duct are removed. Enough of the pancreas is left to make digestive juices and insulin.
After the doctor removes all the cancer that can be seen at the time of the surgery, some patients may receive chemotherapy or radiation therapy to kill any cancer cells that are left. Treatment given after surgery to lower the risk that the cancer will come back is called adjuvant therapy. It is not yet known whether chemotherapy or radiation therapy given after surgery helps keep the cancer from coming back.
The following types of palliative surgery may be done to relieve symptoms caused by a blocked bile duct and improve quality of life:
- Biliary bypass: If cancer is blocking the bile duct and bile is building up in the gallbladder, a biliary bypass may be done. During this operation, the doctor will cut the gallbladder or bile duct in the area before the blockage and sew it to the part of the bile duct that is past the blockage or to the small intestine. This type of surgery creates a new pathway around the blocked area.
- Endoscopic stent placement: If the tumor is blocking the bile duct, surgery may be done to put in a stent (a thin, flexible tube) to drain bile that has built up in the area. The doctor may place the stent through a catheter that drains the bile into a bag on the outside of the body or the stent may go around the blocked area and drain the bile into the small intestine.
- Percutaneous transhepatic biliary drainage: This procedure is used to x-ray the liver and bile ducts. A thin needle is inserted through the skin below the ribs and into the liver. Dye is injected into the liver or bile ducts and an x-ray is taken. If the bile duct is blocked, a stent may be left in the liver to drain bile into the small intestine or a collection bag outside the body.
Radiation therapy
Radiation therapy uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. These are the main ways radiation might be given to treat bile duct cancer:
- External radiation therapy: A machine outside the body sends radiation toward the area of the body with cancer. Radiation is given in a series of treatments to allow healthy cells to recover and to make radiation more effective. The number of treatments is based on details about the cancer, such as the size and location of the tumor.
It is not known whether external radiation therapy helps in the treatment of resectable bile duct cancer. In unresectable, metastatic, or recurrent bile duct cancer, new ways to improve the effect of external radiation therapy on cancer cells are being studied:
- Hyperthermia therapy: Body tissue is exposed to high temperatures to make cancer cells more sensitive to the effects of radiation therapy and certain anticancer drugs.
- Radiosensitizers: Drugs called radiosensitizers make cancer cells more sensitive to radiation therapy. Combining radiation therapy with radiosensitizers may kill more cancer cells.
- Internal radiation therapy: A radioactive substance is sealed in needles, seeds, wires, or catheters that are placed directly into or near the bile duct.
External and internal radiation therapy are used to treat bile duct cancer and may also be used as palliative therapy to relieve symptoms and improve quality of life.
To learn more about radiation therapy and its side effects, see Radiation Therapy to Treat Cancer and Radiation Therapy Side Effects.
Chemotherapy
Chemotherapy uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. There are two main types of chemotherapy used to treat bile duct cancer.
- Systemic chemotherapy: When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body.
Systemic chemotherapy is used to treat unresectable, metastatic, or recurrent bile duct cancer. The following chemotherapy drugs may be used:
- gemcitabine and cisplatin
- capecitabine and oxaliplatin (XELOX)
- gemcitabine and oxaliplatin (GEMOX)
- gemcitabine and capecitabine
- Regional chemotherapy: When chemotherapy is placed directly into an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas.
In unresectable, metastatic, or recurrent bile duct cancer, intra-arterial embolization is being studied. It is a procedure in which the blood supply to a tumor is blocked after anticancer drugs are given in blood vessels near the tumor. Sometimes, the anticancer drugs are attached to small beads that are injected into an artery that feeds the tumor. The beads block blood flow to the tumor as they release the drug. This allows a higher amount of drug to reach the tumor for a longer period of time, which may kill more cancer cells.
It is not known whether systemic chemotherapy helps in the treatment of resectable bile duct cancer.
To learn about the different ways chemotherapy works against cancer, what to expect when receiving chemotherapy, and how to manage chemotherapy side effects, see Chemotherapy to Treat Cancer.
Liver transplant
In a liver transplant, the entire liver is removed and replaced with a healthy donated liver. A liver transplant may be done in patients with perihilar bile duct cancer. If the patient has to wait for a donated liver, other treatment is given as needed.
Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells. Targeted therapies usually cause less harm to normal cells than chemotherapy or radiation therapy do. The following targeted therapies are being studied in patients with bile duct cancer that is locally advanced and cannot be removed by surgery or has spread to other parts of the body:
- ivosidenib
- pemigatinib
- infigratinib
To learn more about how targeted therapy works against cancer, what to expect when having targeted therapy, and targeted therapy side effects, see Targeted Therapy to Treat Cancer.
Immunotherapy
Immunotherapy is a treatment that uses the patient's immune system to fight cancer. Substances made by the body or made in a laboratory are used to boost, direct, or restore the body's natural defenses against cancer.
Immune checkpoint inhibitor therapy is a type of immunotherapy. The following immune checkpoint inhibitor may be used to treat bile duct cancer:
- pembrolizumab
- durvalumab
To learn more about how immunotherapy works against cancer and immunotherapy side effects, see Immunotherapy to Treat Cancer and Immunotherapy Side Effects.
Clinical trials
A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. For some patients, taking part in a clinical trial may be an option.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
To learn more about clinical trials, see Clinical Trials Information for Patients and Caregivers.
Treatment of resectable (localized) bile duct cancer
If the cancer has not spread and is in a place where surgery can be safely done, the tumor and some of the tissue around it will be removed. This lowers the chance of the cancer coming back. Chemotherapy with or without radiation therapy may be given after surgery.
Treatment of resectable intrahepatic bile duct cancer may include the following:
- surgery to remove the cancer, which may include partial hepatectomy with or without embolization before surgery
Treatment of resectable perihilar bile duct cancer may include the following:
- surgery to remove the cancer, which may include partial hepatectomy
- stent placement or percutaneous transhepatic biliary drainage as palliative therapy, to relieve jaundice and other symptoms and improve the quality of life
Treatment of resectable distal bile duct cancer may include the following:
- surgery to remove the cancer, which may include a Whipple procedure
- stent placement or percutaneous transhepatic biliary drainage as palliative therapy, to relieve jaundice and other symptoms and improve the quality of life
Adjuvant therapy for resectable bile duct cancer may include the following:
- chemotherapy
- external-beam radiation therapy
- a clinical trial of adjuvant therapy
Treatment of unresectable bile duct cancer (including metastatic or recurrent disease)
Most people with bile duct cancer cannot have their cancer completely removed with surgery. This may be the case if the cancer has spread too far, the cancer is in a place that is too difficult to completely remove with surgery, or the patient is not healthy enough for surgery.
Treatment of unresectable bile duct cancer (including metastatic or recurrent disease) may include the following:
- stent placement or biliary bypass as palliative treatment to relieve symptoms and improve the quality of life
- external or internal radiation therapy as palliative treatment to relieve symptoms and improve the quality of life
- combination chemotherapy
- an immunotherapy drug
- a clinical trial of various combinations of chemotherapy
- a clinical trial of immunotherapy in patients with mutations (changes) in certain genes
- a clinical trial of targeted therapy in patients with mutations in certain genes
Last Revised: 2023-06-02
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.
