Rheumatoid Arthritis
Condition Basics
What is rheumatoid arthritis (RA)?
Rheumatoid arthritis (RA) is a condition in which the body's own immune system attacks the joints. This causes swollen, stiff, and painful (inflamed) joints, especially in the hands and feet.
Over time, RA can damage and deform joints. It makes it hard to open jars, write, and do other daily tasks. Sometimes it can also cause bumps to form under the skin.
Rheumatoid arthritis is more common in women than in men. It often starts between the ages of 40 and 60.
What causes it?
The cause of RA isn't fully understood. But it's an autoimmune disease. This means that the body's natural defense system attacks the joints. Genes play a role, but experts don't know exactly what that role is.
What are the symptoms?
Symptoms of RA often develop slowly over weeks or months. Fatigue and stiffness are usually early symptoms.
Joint symptoms include:
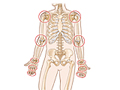
- Pain, stiffness, and swelling in the joints of the hands, wrists, elbows, feet, ankles, knees, or neck. The disease usually affects both sides of the body at the same time.
- Morning stiffness. Joint stiffness may develop after long periods of sleeping or sitting. It usually lasts at least 1 hour and often up to several hours.
- Bumps (nodules). Rheumatoid nodules ranging in size from a pea to a mothball form in nearly one-third of people who have RA. Nodules usually form over pressure points in the body such as the elbows, knuckles, spine, and lower leg bones.
Rheumatoid arthritis can also cause symptoms throughout the body (systemic). These include:
- Fatigue.
- A loss of appetite.
- Weight loss.
- Mild fever.
How is it diagnosed?
To diagnose RA, your doctor looks at a combination of your symptoms and test results. Your doctor will ask you questions about your symptoms and look at your joints for signs of tenderness or swelling.
How is RA treated?
RA is most often treated with medicine. Some medicines help to control the symptoms. Other medicines, especially when used early, can help to prevent the disease from getting worse.
Many of the medicines used to treat rheumatoid arthritis have side effects. Have regular checkups. And talk with your doctor about any problems. This will help your doctor find a treatment that works for you.
Physical therapy and finding the best balance between rest and activity can also help your symptoms.
If your treatment doesn't help, surgery may be an option. The type of surgery you can have depends on which joints are causing problems. Sometimes surgery to replace a joint (such as a hip or knee) is an option. Other types of surgery can remove debris or inflamed tissue from a joint, or relieve pressure on nerves.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
Cause
The cause of RA isn't fully understood. But it's an autoimmune disease. This means that the body's natural defense system attacks the joints.
Genes play a role, but experts don't know exactly what that role is. For most people with RA, the disease doesn't run in their families and they don't pass it along to their children. One or more genes may make it more likely that the body's immune system will attack the tissues of the joints. This immune response may also be triggered by bacteria, a virus, or some other foreign substance.
Symptoms
Symptoms in the joints
RA mostly affects the joints. But it can also cause problems in other parts of your body.
Joint pain can be an early symptom of many different diseases. In RA, symptoms often develop slowly over a period of weeks or months. Fatigue and stiffness are usually early symptoms. Weight loss and a low-grade fever can also occur.
Joint symptoms include:
- Pain, stiffness, and swelling in the joints of the hands, wrists, elbows, feet, ankles, knees, or neck. The disease usually affects both sides of the body at the same time. In rare but severe cases, it may affect the eyes, lungs, heart, nerves, or blood vessels.
- Morning stiffness. Joint stiffness may develop after long periods of sleeping or sitting. It usually lasts at least 1 hour and often up to several hours.
- Bumps (nodules). Rheumatoid nodules ranging in size from a pea to a mothball form in nearly one-third of people who have RA. Nodules usually form over pressure points in the body such as the elbows, knuckles, spine, and lower leg bones.
Symptoms in the neck
When RA affects the joints of the neck, especially the joints at the top of the spine, the bones and joints may dislocate and press on the spinal cord or on the nerve roots. This pressure can cause:
- Neck pain, along with weakness, numbness, or tingling of hands, feet, legs, or arms. This is the most common symptom.
- Loss of bowel or bladder control.
- Unusual head and neck sensations.
Pressure on the spinal cord and nerve roots may obstruct blood flow through the blood vessels in the spinal cord. This compression of the spinal cord is fairly rare. But it can lead to being paralyzed if it's not treated.
Other symptoms
Along with specific joint symptoms, RA can cause symptoms throughout the body (systemic). RA can cause problems in the:
- Eyes. Inflammation of the surface of the eye may cause a dry, gritty-feeling or pain in the eyes.
- Lungs. Inflammation of the membrane sac around the lungs may cause pain and trouble breathing.
- Heart. Thickening and inflammation can occur in the sac around the heart, the heart muscle, and the heart valves. This can cause chest pain and shortness of breath.
- Blood and blood vessels. Low levels of white blood cells and red blood cells and a swollen spleen may occur. Inflammation can affect the blood vessels, causing open skin sores. People with RA seem to develop atherosclerosis earlier than people who don't have RA.
- Nerves and muscles. There may be a loss of strength in muscles next to affected joints. Inflammation may also cause pressure on the nerves.
People with RA may also have fatigue, loss of appetite, weight loss, and a mild fever.
Learn more
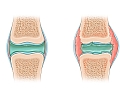
What Happens
The course of RA is hard to predict. It usually progresses slowly, over months or years. In some people it doesn't get worse, and symptoms stay about the same.
RA mostly affects the joints. The inflammation it causes affects the tissues that line the joints, and that can damage and deform the joints. But RA can also cause problems in other parts of the body. It can affect your eyes, lungs, heart, blood vessels, muscles, and nerves. Symptoms can come and go. You may have times in your life when symptoms go away on their own for a while. This is called remission.
If the disease progresses, joint pain can restrict simple movements, such as your ability to grip, and daily activities, such as climbing stairs. It is a common cause of lasting disability. But early treatment may control the disease and keep it from getting worse.
When to Call a Doctor
Call your doctor now if you have:
- Sudden, unexplained swelling and pain in any joint or joints.
- Joint pain along with a fever or rash.
- Pain that is so severe that you can't use the joint.
- Back or neck pain along with weakness in your arms or legs.
- Loss of bowel or bladder control.
Call your doctor within the next few days if you have:
- Joint pain that continues and has not improved for over 6 weeks.
- Side effects that occur with large doses of nonsteroidal anti-inflammatory drugs (NSAIDs) or other medicine used to treat your arthritis. NSAIDs include ibuprofen (Advil) and naproxen (Aleve).
Watchful waiting
Watchful waiting is a wait-and-see approach. It's okay to try home treatment for mild joint pain and stiffness. If there is no improvement after 6 weeks, or if you have any other symptoms, call your doctor.
Early treatment can slow and sometimes prevent significant joint damage.
Exams and Tests
No single lab test can diagnose RA. The doctor will ask you questions about your health and look at your joints for signs of swelling or tenderness. The pattern and nature of joint symptoms are the most important clues to the diagnosis. Your doctor will then rule out other diseases that can cause similar symptoms.
Diagnosis is based on a set of classification criteria. The criteria include the results of these blood tests:
- Anti-cyclic citrullinated peptide antibody (ACPA or anti-CCP) test. It helps confirm the diagnosis and may show your risk of having severe symptoms.
- C-reactive protein. This test may help show how the disease is affecting you.
- Erythrocyte sedimentation rate. It may also help show how the disease is affecting you.
- Rheumatoid factor. This blood test measures the amount of the RF antibody in the blood.
Learn more
Treatment Overview
RA is most often treated with medicine. Physical therapy and finding the right balance between rest and activity can also help. There's no cure for RA, but treatment may help relieve symptoms and control the disease. Treatment usually continues throughout your life. But it will vary depending on:
- The stage. RA may be active or in remission (not having symptoms).
- How severe RA is.
- Your treatment history.
- The benefits and risks of treatment options.
- What you prefer for treatment options. This includes cost, side effects, and daily schedules.
The goal of treatment is to help you maintain your lifestyle, reduce joint pain, slow joint damage, and prevent disability. Treatment should start with learning about the disease. Learn what might happen with joint damage and disability. Find out the risks and benefits of possible treatments. You and your team of doctors can make a long-term treatment plan.
If you try medicine, exercise, and lifestyle changes for at least a few years but pain and disability get much worse, surgery may be an option.
Medicines
Early and ongoing treatment of RA with medicines called disease-modifying antirheumatic drugs (DMARDs) can reduce how severe the disease is. And it can slow or sometimes prevent joints being destroyed. Other medicines may be combined with DMARDs to relieve symptoms. These medicines include:
- Medicines that reduce pain and swelling. Examples are ibuprofen (such as Advil or Motrin) and naproxen (such as Aleve or Naprosyn).
- Medicines that relieve pain. Examples are acetaminophen (Tylenol), codeine, and hydrocodone.
- Corticosteroids. These may be used for early treatment, to control flare-ups, or to help manage the disease.
Treatment options
Types of treatment that may help you control some of the symptoms of RA include:
- Self care. This can include rest, protecting your joints, and healthy eating.
- Physical therapy (PT). This helps improve joint function. PT includes exercise, hot and cold therapy, and massage.
- Occupational therapy. This helps you learn how to maintain movement in the joints while doing the activities of daily life.
- Assistive devices such as household aids or mobility aids. For more information and a catalog, contact the Arthritis Foundation at www.arthritis.org.
- Behavioral modification techniques to reduce pain and stress. They include biofeedback and relaxation therapy, such as breathing exercises and muscle relaxation.
- Counseling. It can help you cope with long-term pain and disability. Counseling can also help if you feel depressed. It's common for people with RA to feel depressed. Also be sure to seek the help and support you need from friends and family members.
- Complementary medicine. It's used by many people with RA to relieve symptoms and improve their quality of life. But there isn't strong scientific evidence that it helps. Therapies include acupuncture, herbs and dietary supplements, and massage.
Surgery
Surgical treatment for RA is used to relieve severe pain and improve function of severely deformed joints that don't respond to medicine and physical therapy. There are several types of surgery that are used. The type of surgery you have depends on which joints are affected. Sometimes surgery to replace a joint (such as a hip or knee) is an option. Other types of surgery can remove debris or inflamed tissue from a joint or can relieve pressure on nerves.
Surgery options include:
- Arthroplasty. This replaces part or all of a joint, such as the hip or knee. Arthroplasty can be done for many different joints in the body. Its success varies depending on which joint is replaced.
- Arthroscopy. This uses a small lighted instrument to remove debris or inflamed tissue from a joint.
- Carpal tunnel release. This surgery relieves pressure on the median nerve in the wrist.
- Cervical spinal fusion. This fusion treats severe neck pain and nerve problems.
- Finger and hand surgeries. These correct joint problems in the hand.
- Foot surgery. An example is phalangeal head resection.
- Synovectomy. This removes inflamed joint tissue.
Learn more
Watch
Self-Care
Living with RA often means making changes to your lifestyle. You can do things at home, such as staying active and taking medicines, to help relieve your symptoms and prevent the disease from getting worse. Here are some ways that you can care for yourself.
- Make time to rest.
RA causes fatigue. And the strain of dealing with pain and limited activities also can make you tired. The amount of rest you need depends on how bad your symptoms are.
- With severe symptoms, you may need long periods of rest. You might need to rest a joint by lying down for 15 minutes several times a day. Try to find a balance between daily activities that you must do or want to do and the amount of rest you need to do those activities.
- Plan your day carefully, and include rest periods. Pace your activities so that you don't get overtired.
- Protect your joints.
You may need to change the way you do certain activities so that you are not overusing your joints. Try to find different ways to relieve your joint pain.
- Joint pain and stiffness may improve with heat therapy, such as:
- Taking warm showers or baths after long periods of sitting or sleeping.
- Soaking hand joints in warm wax baths.
- Sleeping under a warm electric blanket.
- Use assistive devices to reduce strain on your joints. Examples are special kitchen tools or doorknobs.
- Choose the right shoes that fit well and will not cause joint problems.
- Use splints, canes, or walkers to reduce pain and improve function.
- Joint pain and stiffness may improve with heat therapy, such as:
- Stay active.
Keep moving to keep your muscle strength, flexibility, and overall health.
- Physical therapy may be recommended by your doctor.
- Exercise for arthritis takes three forms—stretching, strengthening, and conditioning. Exercise can improve or maintain quality of life for people who have RA. Your specific joint problem may guide the type of activity that will help the most. For example:
- Swimming is a good activity if you have joint problems in your knees, ankles, or feet.
- Bicycling and walking are good activities if your joint problems are not in your legs or feet.
- Avoid smoking.
People with RA have an increased risk of plaque in the arteries (atherosclerosis). Smoking increases this risk even more. Smoking may also lower your response to treatment.footnote 1 So, if you smoke, quit.
- Eat healthy foods.
Try to eat a variety of healthy foods. Dietary needs are not the same for all people who have RA. To be sure you get the nutrients you need, you can ask a registered dietitian to help you make a plan.
- Be sure to get enough calcium and vitamin D to protect your bones against osteoporosis.
- Lose weight, if you are overweight.
- People who have rheumatoid arthritis also have an increased risk of heart disease. But healthy lifestyle changes, such as exercise and a healthy diet, may reduce your risk.
- Take care of your teeth and gums.
People who have RA tend to get gum disease. You can help prevent gum disease through good basic dental care.
Exercise to help reduce pain
Exercise can reduce pain and improve function in people who have RA. It may also help prevent the buildup of scar tissue. This can lead to weakness and stiffness. Exercise for arthritis takes three forms:
- Stretching.
Stretching involves moving joint and muscle groups through and slightly beyond their normal range of motion and holding them in position for at least 15 to 30 seconds.
- Strengthening.
Strengthening involves moving muscles against some resistance. Strengthening exercise helps people who have RA stay more active and able to do their daily activities. It even seems to help their outlook.footnote 1
- Conditioning.
Conditioning exercise improves aerobic fitness. It may help reduce pain and help you stay more active.footnote 2 Even moderate activity, such as walking, can improve your health and may prevent disability from RA.
Be sure to follow your doctor's advice about your exercise program.
Learn more
Watch
Medicines
Medicines are the main treatment for RA. The types of medicines used, the amount you take, and the length of time you take them depends on how severe your RA is, how fast it's progressing, and how it affects your daily life.
Medicines are used to:
- Relieve or reduce pain.
- Improve daily function.
- Reduce joint inflammation.
- Prevent or delay serious joint damage and deformity.
- Prevent lasting disability.
- Improve quality of life.
Medicines called disease-modifying antirheumatic drugs (DMARDs) can slow or sometimes prevent joints from being destroyed. An early start to treatment with DMARDs can reduce how severe RA is. These medicines are most often taken over a long period to help control the disease.
Other medicines may be combined with DMARDs to relieve symptoms. They include:
- Medicines that reduce pain and swelling. These include aspirin, ibuprofen, and naproxen.
- Corticosteroids. An example is prednisone.
- Medicines that relieve pain. These include acetaminophen, acetaminophen combined with codeine or hydrocodone, and tramadol.
Learn more
Watch
Surgery
Surgical treatment for RA is used to relieve severe pain and improve function of severely deformed joints that don't respond to medicine and physical therapy.
Surgery options include:
- Arthroplasty. This replaces part or all of a joint, such as the hip or knee. It can be done for many different joints in the body. How well it works depends on which joint is replaced.
- Arthroscopy. This uses a small lighted tool to remove debris or inflamed tissue from a joint.
- Carpal tunnel release. It relieves pressure on the median nerve in the wrist.
- Cervical spinal fusion. It treats severe neck pain and nerve problems.
- Finger and hand surgeries. They correct joint problems in the hand.
- Foot surgery. An example is phalangeal head resection.
- Synovectomy. It removes inflamed joint tissue.
Learn more
References
Citations
- O'Dell JR (2013). Treatment of rheumatoid arthritis. In GS Firestein et al., eds., Kelley's Textbook of Rheumatology, 9th ed., vol. 2, pp. 1137–1160. Philadelphia: Saunders.
- Baillet A, et al. (2010). Efficacy of cardiorespiratory aerobic exercise in rheumatoid arthritis: Meta-analysis of randomized controlled trials. Arthritis Care and Research, 62(7): 984–992.
Credits
Current as of: July 10, 2023
Author: Healthwise Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: July 10, 2023
Author: Healthwise Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.