Introduction
Stroke is the third most common cause of death, after heart disease and cancer, in the United States. There are approximately 700,000 cases of stroke every year in this country and nearly 175,000 patients die from stroke or its associated complications each year. A stroke is defined as the sudden interruption or severe reduction of blood supply to part of the brain. This deprives the brain tissue of necessary oxygen and nutrients causing brain cells to die within minutes of the stroke’s onset. A transient ischemic deficit (TIA), or “mini stoke,” results from a temporary interruption of blood flow to the brain and symptoms typically last less than 15 minutes but can last up to 24 hours. A TIA can be a precursor of a larger stroke. There are two main types of strokes: Ischemic (resulting from decreased blood flow to the brain) and hemorrhagic (from bleeding into the brain). Ischemic strokes are far more common than hemorrhagic strokes.
Risk Factors
There are several risk factors for stroke, including deposition of fat within the arterial walls and hardening of the arteries (atherosclerosis), high blood pressure, smoking, diabetes, certain heart conditions, and diseases that cause the blood to clot too quickly.
Symptoms
Symptoms of stroke can be distinctive. The clinical deficit or neurological impairment depends on the location and extent of the arterial occlusion. Common signs and symptoms of a stroke may include sudden:
- Numbness or weakness of the face, arm or leg especially on one side
- Confusion or dizziness
- Trouble speaking or understanding
- Trouble seeing in one or both eyes
- Trouble walking, loss of balance or coordination
- Severe headache with no known cause
- Trouble swallowing
The patient may also experience sudden loss of consciousness and seizures. If you or anyone you know experiences these symptoms, emergency medical care should be sought. It is imperative for the patient to reach the hospital as quickly as possible for certain types of treatments to be successful.
Diagnosis
The diagnosis of stroke can often be easily made by history taking and examination. However, an emergent workup with laboratory and imaging evaluation is often required to plan further treatment. The imaging evaluation in the ER often includes a CT scan and/or an MRI of the brain. Using CT and MRI, a radiologist can not only distinguish between the ischemic and hemorrhagic strokes but can also determine the extent of damage to the brain parenchyma. Moreover, using newer techniques, we can now estimate the amount of brain that can be saved if clot lysis (clot busting) can be started in time (within 3-6 hours of symptom onset).
Treatment
At the University of Michigan, we adopt a multi-disciplinary approach to stroke treatment. Our team of physicians consists of emergency medicine physicians, neurologists, neurosurgeons, and interventional neuroradiologists. Whenever a patient with a stroke is admitted to the emergency room, everyone in the stroke team is alerted and based upon imaging studies and timing, a decision is made whether to intervene. The treatment of a stroke victim involves several issues including:
- Management in the acute phase.
- Measures to restore flow to the brain.
- Physical therapy and rehabilitation.
- Measures to prevent further strokes in the future.
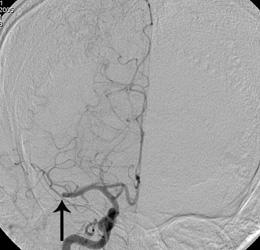
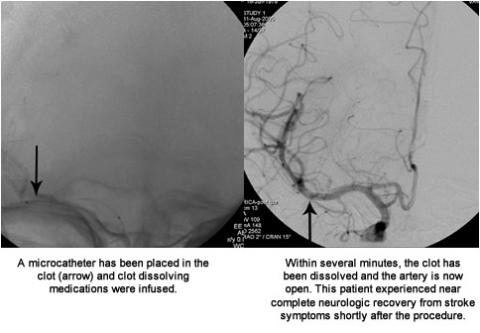
Restoration of the blood flow to the brain
If the patient gets to the hospital within 3-6 hours of stroke onset, they may be candidates for receiving clot-dissolving medications. These medicines can cause the stroke symptoms to stop or reverse very quickly. These medications can also prevent long-term disability or death. If the patient gets to the hospital within 3 hours of stroke onset, these clot dissolving medications can be administered intravenously. However, if more than three (but less than six) hours have passed from the stroke onset, this medication needs to be delivered intra-arterially within the clot itself. Our advanced state-of-the-art equipment, with two dedicated biplane neuroangiography suites, gives us the capability to care for stroke patients requiring interventional (intra-arterial) therapy 24-hours-a-day, 7-days-a-week. Our team of interventional neuroradiologists and endovascular neurosurgeons is available round the clock for such treatments. Endovascular procedures are usually performed, from the groin area. A long small tube called catheter, is placed into an artery or vein and navigated through the blood vessels to the site of the problem. In the case of a stroke, the catheter is placed as close to the clot or thrombus as possible. Once at the site, check angiograms are performed to ensure correct placement of the catheter and the following options for treatment are then available:
Clot dissolving agents
Intra-arterial tissue plasminogen activators (most frequently tPA) can help in dissolution of the blood clots. This drug is infused within the clot by the interventional neuroradiologist. Intermittent angiograms are performed to demonstrate the extent of clot dissolution.
Merci Clot Retrieval System
The Merci clot retrieval system is a new, mechanical device that is shaped similar to a “corkscrew.” Through a microcatheter, this small flexible device is passed through the clot. The device is then allowed to unwind and lodges itself within the clot. After the device is deployed within the clot, the device is slowly withdrawn into from the artery, bringing the clot with it.
Stenting and Angioplasty
Sometimes, arterial blockages or clots are associated with underlying atherosclerotic narrowing of the vessels. These areas of narrowing can be treated with stenting and angioplasty. A small puncture is made in the femoral artery in your groin area under local anesthesia. A guiding catheter is advanced under x-ray guidance into the internal carotid artery. A small caliber wire is then negotiated under x-ray guidance past the area of narrowing. A stent is then positioned across the narrowed area in the artery within the brain. The stent is released and then dilated with an angioplasty balloon. The stent stays in place permanently holding the artery open and improving blood flow. The stent also holds the plaque against the artery wall. This reduces the risk of plaque breaking off, traveling to your brain, and causing a stroke. Most stents are made from nickel-titanium, a metal that is bendable but springs back into its original shape after being bent. A vascular closure device may be used to close the small incision in your groin or pressure applied to the puncture site until bleeding stops. These additional procedures can be performed at the same sitting or separately depending on the clinical situation. 

