Type 1 Diabetes
Condition Basics
What is type 1 diabetes?
Type 1 diabetes is a disease that starts when the pancreas stops making enough of a hormone called insulin. Insulin helps the body use sugar from food as energy or store it for later use. If there isn't any insulin, too much sugar stays in the blood. Over time, high blood sugar can harm many parts of the body. These include the eyes, heart, blood vessels, nerves, and kidneys.
Type 1 diabetes can occur at any age, but it usually starts in children or young adults. It's a lifelong disease. But with treatment and a healthy lifestyle, people can live a long and healthy life.
What causes it?
The body makes insulin in beta cells, which are in a part of the pancreas called the islet (say "EYE-let") tissue. Type 1 diabetes starts because the body's immune system destroys those beta cells. So people who have type 1 diabetes can't make their own insulin.
What are the symptoms?
Symptoms of type 1 diabetes include urinating often, being very thirsty, losing weight without trying, being hungrier than usual, and having blurry vision. Symptoms are caused by high blood sugar. They usually develop quickly, over a few days to weeks. At first, symptoms may be overlooked or mistaken for another illness, like the flu.
How is it diagnosed?
The doctor will ask about past health issues and do a physical exam. Blood tests are done to measure how much sugar is in the blood. The doctor will use those blood test results and the American Diabetes Association criteria to diagnose diabetes.
How is type 1 diabetes treated?
Treatment for type 1 diabetes focuses on keeping blood sugar levels within a target range and doing things to reduce complications. Taking insulin, making healthy food choices, and getting regular exercise can help control blood sugar. You'll also need to check blood sugar levels several times a day.
How can you prevent the complications of diabetes?
You can help prevent or delay complications by keeping your blood sugar in a target range. You also need regular medical checkups to look for early signs of complications. If complications are treated early, the damage may be stopped, slowed, or possibly reversed.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
What Increases Your Risk
Risk factors are things that increase the chances of getting sick or having a problem. Risk factors for type 1 diabetes include:
- Family history. A family history of type 1 diabetes increases the chance of a person having autoantibodies such as islet cell antibodies. These antibodies attack the cells in the pancreas that produce insulin. But a family history of type 1 diabetes doesn't mean that someone will definitely have the disease.
- Presence of autoantibodies in the blood. People who have both a family history of type 1 diabetes and two or more autoantibodies in their blood are likely to get type 1 diabetes. If a person has family members with type 1 diabetes, the person can be tested to look for autoantibodies.
- Race. White people have a greater risk for type 1 diabetes than Black, Asian, or Hispanic people.
Prevention
Currently there is no way to prevent type 1 diabetes. But studies are looking into ways to prevent it in those who are most likely to get it. If you have a parent, brother, or sister with type 1 diabetes, and you're willing to take part in a study, talk to your doctor.
Symptoms
Symptoms of type 1 diabetes are caused by high blood sugar. They usually develop quickly, over a few days to weeks. At first, symptoms may be overlooked or mistaken for another illness, like the flu.
Symptoms include:
- Urinating often. This may be more noticeable at night.
- Being very thirsty. This happens if a person urinates so often that they get dehydrated.
- Losing weight without trying. This happens because the body isn't able to get energy from sugar. Instead, the body uses muscle and fat for energy.
- Increased hunger. The body isn't using all the calories that it can. Many calories leave the body through urine.
- Blurry vision. When sugar builds up in the lens of the eye, it sucks extra water into the eye. This changes the shape of the lens and blurs vision.
- Feeling very tired. The body isn't using the calories it takes in, and it isn't getting the energy it needs.
Symptoms of high and low blood sugar
You have most symptoms of type 1 diabetes when your blood sugar is either too high or too low.
Common symptoms of high blood sugar include:
- Thirst.
- Needing to urinate often.
- Weight loss.
- Blurry vision.
Common symptoms of low blood sugar include:
- Sweating.
- Shakiness.
- Weakness.
- Hunger.
- Confusion.
If you wait too long to get medical care when your blood sugar goes too high, you may develop diabetic ketoacidosis. Symptoms include:
- Flushed, hot, dry skin.
- A strong, fruity breath odor.
- Feeling restless or drowsy, or having trouble waking up.
- Lack of interest in normal activities.
- Rapid, deep breathing.
- Loss of appetite, belly pain, and vomiting.
- Confusion.
Learn more
What Happens
Over time, high blood sugar can lead to serious problems. It can:
- Harm your eyes, nerves, and kidneys.
- Damage your blood vessels, leading to heart disease and stroke.
- Reduce blood flow and cause nerve damage to parts of your body, especially your feet. This can cause slow healing and pain when you walk.
That's why it's important to keep your blood sugar within a target range.
A more sudden problem can happen when the blood sugar level gets so high that a serious chemical imbalance develops in the blood. This condition can be life-threatening and needs quick treatment.
When people hear the word "diabetes," they often think of problems like these. But daily care and treatment can help prevent or delay these problems. The goal is to keep your blood sugar in a target range. It's the best way to reduce your chance of having more problems from diabetes.
Learn more
When to Call a Doctor
Call 911 or other emergency services immediately if:
- You have symptoms of diabetic ketoacidosis (DKA), such as:
- Blurred vision.
- Trouble staying awake or trouble being woken up.
- Fast, deep breathing.
- Breath that smells fruity.
- Belly pain, not feeling hungry, and vomiting.
- Feeling confused.
- You passed out (lost consciousness), or if you suddenly become very sleepy or confused. (You may have very low blood sugar, called hypoglycemia.)
Call a doctor now if:
- You are sick and can't manage your blood sugar. Your doctor may have given you instructions on how to manage your blood sugar when you are sick.
- You have been vomiting or have had diarrhea for more than 6 hours.
- You have a blood sugar level that stays higher than the level the doctor has set for you (for example, 300 milligrams per deciliter (mg/dL) for two or more readings).
- You have blood sugar that stays lower than the level the doctor has set for you (for example, 70 mg/dL for two or more readings).
- You have symptoms of low blood sugar, such as:
- Sweating.
- Feeling nervous, shaky, and weak.
- Extreme hunger and slight nausea.
- Dizziness and headache.
- Blurred vision.
- Confusion.
Check with your doctor if:
- You often have problems with high or low blood sugar levels.
- You have trouble knowing when your blood sugar is low (hypoglycemia unawareness).
- You have questions or want to know more about diabetes.
- You are planning to get pregnant in the next year.
- You don't want to get pregnant, so you can talk with your doctor about birth control options.
Planning pregnancy when you have type 1 diabetes
If you are planning to become pregnant, talk to your doctor about making sure that your blood sugar is well-managed.
High blood sugar levels during the first trimester of pregnancy raise the risk of birth defects. Good care of diabetes before conception appears to reduce the risk of birth defects.
Learn more
Exams and Tests
The doctor will ask about past health issues and do a physical exam. Blood tests are done to measure how much sugar is in the blood. The doctor will use those test results and the American Diabetes Association criteria to diagnose diabetes.
Some people are diagnosed with type 1 diabetes because they have symptoms of diabetic ketoacidosis.
It may be hard to tell what type of diabetes a person has. If so, the doctor may do a C-peptide test or test for autoantibodies to diagnose type 1 diabetes or a slowly developing form of type 1 diabetes called latent autoimmune diabetes in adults (LADA). Some rare forms of diabetes are caused by a genetic problem. Genetic testing may be done to diagnose them. This includes maturity onset diabetes of the young (MODY). There are many types of MODY, depending on the gene that is affected.
Tests to check your health and screen for problems
Tests you may have include:
- A1c blood test.
This shows whether your blood sugar has been staying within your target range.
- Blood pressure test.
High blood pressure can damage nerves and blood vessels.
- Cholesterol test.
High cholesterol raises the risk for heart attack and stroke.
- Albumin-creatinine ratio test.
This checks for protein in the urine, a sign of kidney damage.
- Blood creatinine test/estimated glomerular filtration (eGFR).
This shows how well your kidneys are working.
- Complete foot exam.
The doctor checks for foot sores and loss of sensation.
- Dental exam and cleaning.
The dentist checks for gum disease and tooth decay.
- Complete eye exam.
This checks for damage to the back of the eye (diabetic retinopathy).
- Thyroid-stimulating hormone (TSH) blood test.
This checks for thyroid disease.
Learn more
- A1c Test
- Albumin Urine Test
- Blood Glucose Test
- Blood Pressure Screening
- Cholesterol and Triglycerides Tests
- C-Peptide Test
- Creatinine and Creatinine Clearance Tests
- Criteria for Diagnosing Diabetes
- Diabetes: Blood Sugar Levels
- Diabetes: Checking Your Feet
- Diabetes: Tests to Watch for Complications
- Dilated Eye Exam
- Glomerular Filtration Rate (GFR)
- Thyroid-Stimulating Hormone (TSH) Test
Treatment Overview
Treatment for type 1 diabetes focuses on keeping blood sugar levels within a target range. This will help prevent problems from diabetes such as eye, kidney, heart, and nerve disease.
To manage type 1 diabetes, a person will:
- Take insulin every day. This may be done through an insulin pump or a syringe (needle).
- Check blood sugar levels often.
- Make healthy food choices.
- Get regular physical activity. Exercise helps the body to use insulin in a more efficient way.
- Get routine screening tests and exams. These are done to watch for signs of problems.
- Avoid smoking.
Blood sugar levels are easier to manage when mealtimes, amount of food, and exercise are similar every day.
Medicine to treat other health problems, like high blood pressure or high cholesterol, may be needed. This may help prevent problems from diabetes.
Self-Care
Here are some things you can do to care for yourself:
- Take your insulin on time and in the right dose.
- Check and record your blood sugar as often as directed by your doctor. Keep track of any symptoms you have.
- Follow your meal plan to know how much carbohydrate to eat at each meal and snack.
- Check your feet daily for blisters, cracks, and sores.
- Get a checkup every 3 to 6 months. Your doctor will tell you how often to come in.
- Aim for 30 minutes of exercise on most, preferably all, days of the week.
- Control your cholesterol and blood pressure. Exercise and healthy eating can help. If you have medicine for cholesterol or high blood pressure, take it as directed.
- If your doctor say it's okay, take a low-dose aspirin every day to help prevent heart attack and stroke.
- If you smoke, quit. Ask your doctor about stop-smoking programs and medicines.
Learn more
Watch
Medicines
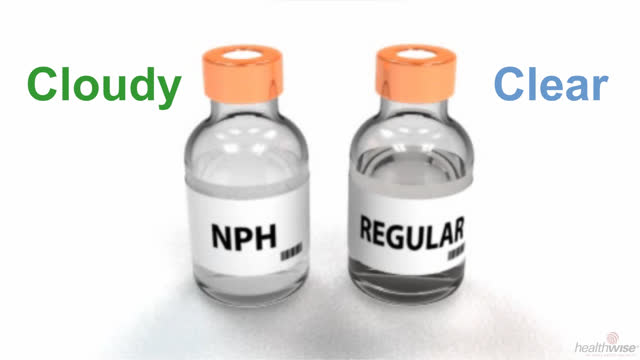
Insulin helps keep your blood sugar level within a target range. It can be taken as a shot (injection) or through an insulin pump. Rapid-acting insulin is also available as a powder that you inhale.
Most people who have type 1 diabetes take a combination of types of insulin. For instance, they may take a long-acting insulin once or twice a day and a rapid-acting insulin before each meal. The amount and type of insulin needed varies for each person.
- The amount and type of insulin you need changes over time. It depends on your age, hormones (such as during rapid growth or pregnancy), and changes in exercise routine.
- You may need higher doses during times of illness or emotional stress.
Never skip a dose of insulin without the advice of your doctor.
Learn more
Watch
Surgery
Surgery may be an option for certain people who have type 1 diabetes. Choices may include:
- Pancreas transplant.
When insulin isn't enough to keep blood sugar in your target range, a pancreas transplant might be an option. If it's successful, you may no longer have symptoms or need to treat diabetes. But you may still get complications from diabetes. And you must take medicine to keep your body from rejecting the new organ.
- Pancreatic islet cell surgery.
This involves inserting a small group of donated pancreas cells (islet cells) through a vein in your liver. After surgery, these cells start to make insulin. If they can make enough, you may no longer need insulin injections. But you must take medicine to prevent rejection.
Watch
Getting Support
Finding the right support can take a little time and effort. But it can be worth it. You'll feel more connected to others, and that connection can really help you manage your diabetes.
- Surround yourself with people who have similar goals.
For example, if you want to be more active, try to spend time with people who also want to be more active.
- Try a support group.
Support groups aren't for everyone. But they can be a great source of connection and inspiration.
- Let others know what you need.
You may have to help others know how they can help.
- If it's hard to ask for what you need, try writing down what you'll say first.
- Give others specific ideas. For example, "I feel bad about myself when you say I shouldn't drink soda. It would help me if we didn't have it around."
- Ask yourself some questions.
You may want to take a little time to write down your answers to these questions.
- What would be the good things about getting support?
- What people in your life might support you?
- What might be people's reactions when you ask for support? How will you respond?
- How and when will you ask for support?
Learn more
Watch
Credits
Current as of: October 2, 2023
Author: Healthwise Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: October 2, 2023
Author: Healthwise Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
 Insulin pump
Insulin pump Pancreas transplant
Pancreas transplant Diabetes: How Testing Helps You Stay In Your Range
Diabetes: How Testing Helps You Stay In Your Range Diabetes: Insulin's Role
Diabetes: Insulin's Role Diabetes: Testing Your Blood Sugar
Diabetes: Testing Your Blood Sugar How to Give a Glucagon Shot
How to Give a Glucagon Shot How to Use an Insulin Pen
How to Use an Insulin Pen How to Use Glucagon Nasal Spray
How to Use Glucagon Nasal Spray Learning About Glucagon
Learning About Glucagon Learning About Insulin Pens
Learning About Insulin Pens Type 1 Diabetes in Children: Bryson's Story
Type 1 Diabetes in Children: Bryson's Story Type 1 Diabetes in Children: How to Support Your Teen
Type 1 Diabetes in Children: How to Support Your Teen What Is Type 1 Diabetes?
What Is Type 1 Diabetes?
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.