Skin Cancer, Melanoma
Condition Basics
What is melanoma?
Melanoma is a kind of skin cancer in which abnormal skin cells grow out of control. It isn't as common as other types of skin cancer, but it is the most serious because it can spread quickly to other parts of the body.
Most melanomas show up as a new spot or skin growth. But they can also form in an existing mole or other mark on the skin. A melanoma usually looks like a flat mole with uneven edges and a shape that isn't the same on both sides. It may be black, brown, or more than one color. Less often, melanoma begins in other places, such as the eye or the intestines. In people with darker skin, some of the most common sites are the palms of the hands, the soles of the feet, or underneath the nails.
What causes it?
Too much UV radiation from sun exposure can damage DNA. This can cause normal skin cells to become abnormal. These abnormal cells can quickly grow out of control. Having lighter skin, a family history of melanoma, or many abnormal moles puts you at higher risk for this disease.
What are the symptoms?
You may not have any symptoms in the early stages of melanoma. Or a melanoma may be sore, or it may itch or bleed. Most melanomas start as a new skin growth. But any change in the shape, size, or color of a mole may be a sign of melanoma.
Source: NCI Visuals Online. Skin Cancer Foundation. www.cancer.gov.
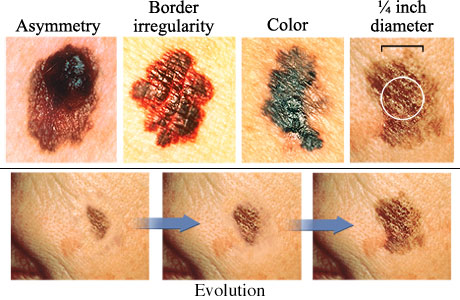
The ABCDEs of melanoma skin cancer are:
- Asymmetry. One half doesn't match the appearance of the other half.
- Border irregularity. The edges are ragged, notched, or blurred.
- Color. The color (pigmentation) is not uniform. Shades of tan, brown, and black are present. Dashes of red, white, and blue add to a mottled appearance.
- Diameter. The size of the mole is greater than 1/4 inch (6 mm), about the size of a pencil eraser. Any growth of a mole should be evaluated.
- Evolution. There is a change in the size, shape, symptoms (such as itching or tenderness), surface (especially bleeding), or color of a mole.
How is it diagnosed?
Your doctor will check your skin for melanoma. If your doctor suspects melanoma, a sample of tissue (biopsy) will be removed and tested. If your biopsy shows melanoma, you may have more tests to find out if it has spread to your lymph nodes or other places.
How is melanoma treated?
Treatment for melanoma is based on the stage of the cancer and other things, such as your overall health. The main treatment is surgery to remove the cancer. Other treatment options may include immunotherapy and targeted therapy. In some cases, chemotherapy and radiation therapy may be used.
How can you lower your risk?
The best way to lower your risk for melanoma is to protect your skin whenever you are out in the sun. For example, stay out of the sun during midday hours. Wear sun-protective clothes. Use sunscreen with an SPF of at least 30 every day. Avoid sunbathing and tanning salons.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
Cause
What exactly causes melanoma isn't known. But some things, like too much UV radiation from sun exposure, can damage DNA. This can cause normal skin cells to become abnormal. These abnormal cells can quickly grow out of control.
Any of these things can put you at higher risk for this disease:
- Getting sunburns, especially during childhood.
- Spending too much time in the sun.
- Using tanning beds or sunlamps.
- Having lighter skin. But people with any skin color can get melanoma.
- Having a family history of melanoma.
- Having many abnormal, or atypical, moles. These moles may fade into the skin and have a flat part that is level with the skin. They may be smooth or slightly scaly. Or they may look rough and "pebbly."
Learn more
Lowering Your Risk
The best way to lower your risk for melanoma is to protect yourself whenever you are out in the sun.
- Try to stay out of the sun during the middle of the day (from 10 a.m. to 4 p.m.).
- Wear sun-protective clothes, such as a hat that shades your face, a long-sleeved shirt, and long pants.
- Use sunscreen every day.
- Your sunscreen should have an SPF of at least 30 and protect against both UVA and UVB radiation.
- Reapply sunscreen every 2 hours.
- Take extra care to protect your skin when you're near water, at higher elevations, or in tropical climates.
- Avoid sunbathing and tanning salons.
Check your skin regularly for odd marks, moles, or sores that won't heal. Pay extra attention to areas that get a lot of sun, such as your hands, arms, and back.
Learn more
Watch
Symptoms
You may not have any symptoms in the early stages of melanoma. Or a melanoma may be sore, or it may itch or bleed.
Most melanomas start as a new skin growth on unmarked skin. The growth may change color, shape, or size. These types of changes are an early sign that the growth is melanoma.
But melanoma can also develop in an existing mole or other mark on the skin. Or it may look like a bruise that isn't healing. Or it might show up as a brown or black streak under a fingernail or toenail.
Melanoma can grow anywhere on the body.
- It often occurs on the back, head and neck, or arms and legs.
- In older people, the face, neck, scalp, and ears are common places for melanoma to grow.
- Melanoma can grow in other places. These include the soles of the feet, the palms of the hands, and nail beds. These sites are most common for people with darker skin. Melanoma can also occur on mucous membranes, such as the mouth or the intestines.
Signs of melanoma
The most important warning sign for melanoma is any change in size, shape, or color of a mole or other skin growth, such as a birthmark. Watch for changes that occur over a period of weeks to a month. The ABCDE system tells you what changes to look for.
- A for asymmetry. One half of the mole or skin growth doesn't match the other half.
- B for border irregularity. The edges are ragged, notched, or blurred.
- C for color. The color isn't the same throughout the mole.
- D for diameter. The mole or skin growth is larger than the size of a pencil eraser.
- E for evolution. There is a change in the size, shape, symptoms (such as itching or tenderness), surface (especially bleeding), or color of a mole.
Signs of melanoma in an existing mole
Signs of melanoma in an existing mole include changes in:
- Elevation, such as thickening or raising of a previously flat mole.
- Surface, such as scaling, erosion, oozing, bleeding, or crusting.
- Surrounding skin, such as redness, swelling, or small new patches of color around a larger lesion (satellite pigmentations).
- Sensation, such as itching, tingling, burning, or pain.
- Consistency, such as softening or small pieces that break off easily.
Metastatic melanoma
With metastatic melanoma, the symptoms may be vague. And any symptoms will likely depend on where the melanoma has spread in the body. Symptoms may include swollen or painful lymph nodes, lumps under the skin, an ongoing cough, swelling or pain in the belly, headaches, or unexplained weight loss.
What Happens
Melanoma develops when normal cells that produce pigment become abnormal and grow out of control. Then these cells invade surrounding tissues. Melanomas can begin in an existing mole or other skin growth. But most start in unmarked skin.
Melanoma can spread (metastasize). It most often spreads first into nearby lymph nodes. It can also spread through the bloodstream to the skin, liver, lungs, bone, and brain.
When melanoma is found early, it can often be cured by surgery to remove it. But after melanoma spreads, it is harder to cure.
Learn more
When to Call a Doctor
Call your doctor now if you have any of these symptoms:
- You have trouble breathing or swallowing.
- You cough up or spit up blood.
- You have blood in your vomit or stool (bowel movement).
- Your urine or stool is black, and the blackness isn't caused by taking iron or Pepto-Bismol.
The most important warning sign for melanoma is a change in size, shape, or color of a mole or other skin growth (such as a birthmark). Call your doctor if you have:
- Any change in a mole, including size, shape, color, soreness, or pain.
- A bleeding mole.
- A discolored area under a fingernail or toenail not caused by an injury.
- A general darkening of the skin unrelated to sun exposure.
If you have been diagnosed with cancer, be sure to follow your doctor's instructions about calling when you have problems, new symptoms, or symptoms that get worse.
Exams and Tests
To check for melanoma, your doctor may:
- Ask you about your medical history and your family history.
- Do a physical exam. This will include checking your skin to look for melanoma.
- Do a skin biopsy. Your doctor will take a sample of your skin and have it tested for melanoma.
- Check your lymph nodes to see if they are larger than normal. This may be followed by a sentinel lymph node biopsy to see if the melanoma has spread to your lymph system.
- Do imaging tests. These tests include PET scan, CT scan, and MRI. These tests can show if the cancer has spread to other parts of your body, such as the lungs, brain, or liver.
Other techniques may include total-body photography. A series of photos of the suspicious lesions may be taken. These photos can be used as a baseline to compare with follow-up photos.
Screening tests for skin cancer
Skin cancer may be treated more successfully if it is caught early.
- The U.S. Preventive Services Task Force (USPSTF) hasn't recommended for or against routine skin cancer screening for adults at normal risk.footnote 1 This means the USPSTF didn't find enough evidence from studies to show that all adults with a normal risk for skin cancer would benefit from having regular screening.
- But your doctor may suggest a regularly scheduled skin exam if your risk is higher than average because you have:
- Abnormal moles called atypical moles (dysplastic nevi). These moles are not cancerous, but their presence could be a sign of an inherited tendency to develop melanoma.
- Increased occupational or recreational exposure to ultraviolet (UV) radiation.
- Familial atypical multiple mole and melanoma (FAMMM) syndrome. This is an inherited tendency to develop melanoma. People that have it may need to check their skin every month and be checked by a doctor several times a year.
Learn more
Watch
Treatment Overview
Treatment for melanoma is based on the stage of the cancer and other things, such as your overall health. The main treatment is surgery to remove the cancer. Other treatment options may include immunotherapy and targeted therapy.
If melanoma has spread beyond the skin (metastatic cancer), you may have surgery. You'll probably need other treatments too. These may include immunotherapy or targeted therapy. In some cases, radiation therapy or chemotherapy may be used.
Your doctor will talk with you about your options and then make a treatment plan.
Surgery
The doctor removes the cancer and a border of normal skin (margin) around it. If you have early-stage cancer, the doctor may be able to remove all of it. You may not need more treatment.
If a large melanoma is removed, you may need a skin graft or other repair surgery.
In some cases, one or more lymph nodes may be removed.
- The doctor may remove the first lymph node that the cancer may have spread to. This is called a sentinel lymph node biopsy. If no cancer cells are found, you may not need to have more lymph nodes removed.
- If cancer is found in the sentinel lymph node, nearby lymph nodes may be removed and checked for cancer cells.
After surgery, you may have only regular checkups. Or you may also have other treatments to help prevent a return (recurrence) of the cancer.
Medicines
Medicines used to treat melanoma include:
- Immunotherapy. This treatment helps your immune system fight cancer. The medicine may be spread on the melanoma or injected into it. Or it may be injected into a vein or under the skin.
- Targeted therapy. These medicines target cancer cells and may cause less harm to normal cells. They help keep cancer from growing or spreading. Some of these medicines target a specific gene in the cancer cells. If you have a gene that can be targeted, you may be given one or more of these medicines. They are usually given as pills.
Treatment for metastatic or recurrent cancer
Melanoma that has spread to other parts of the body (metastatic cancer) may cause tumors. These can sometimes be removed with surgery. But metastatic melanoma often needs other treatments too. Examples include immunotherapy, targeted therapy, and chemotherapy. These treatments and others may also be used for melanoma that has come back after treatment (recurrent cancer).
Radiation therapy may help relieve symptoms caused by melanoma that has spread to the bones or other organs. Radiation therapy uses high-dose X-rays to destroy cancer cells and shrink tumors.
Clinical trials are research studies that test new treatments to find out how well they work. Your medical team can tell you if there's a clinical trial that might be right for you.
Learn more
Watch
Supportive Care
Palliative care is a type of care for people who have a serious illness. It's different from care to cure your illness, called curative treatment. Palliative care provides an extra layer of support that can improve your quality of life—not just in your body, but also in your mind and spirit. Sometimes palliative care is combined with curative treatment.
The kind of care you get depends on what you need. Your goals guide your care. You can get both palliative care and care to treat your illness. You don't have to choose one or the other.
Palliative care can help you manage symptoms, pain, or side effects from treatment. It may help you and those close to you better understand your illness, talk more openly about your feelings, or decide what treatment you want or don't want. It can also help you communicate better with your doctors, nurses, family, and friends.
End-of-life care
It can be hard to live with an illness that cannot be cured. But if your health is getting worse, you may want to make decisions about end-of-life care. Planning for the end of your life does not mean that you are giving up. It is a way to make sure that your wishes are met. Clearly stating your wishes can make it easier for your loved ones. Making plans while you are still able may also ease your mind and make your final days less stressful and more meaningful.
Learn more
Watch
Self-Care
- Learn the most important warning signs for melanoma—a change in the size, shape, or color of a mole or other skin growth, such as a birthmark.
- Check all the skin on your body once a month for skin growths or other changes, such as changes in color and feel of the skin.
- Stand in front of a full-length mirror. Look carefully at the front and back of your body. Then look at your right and left sides with your arms raised.
- Bend your elbows and look carefully at your forearms, the back of your upper arms, and your palms.
- Look at your feet, the bottoms of your feet, and the spaces between your toes.
- Use a hand mirror to look at the back of your legs, the back of your neck, and your back, rear end (buttocks), and genital area. Part the hair on your head to look at your scalp.
- If you see a change in a skin growth, contact your doctor. Look for:
- A mole that bleeds.
- A fast-growing mole.
- A scaly or crusted growth on the skin.
- A sore that will not heal.
- Take your medicines exactly as prescribed. Call your doctor if you think you are having a problem with your medicine.
- If you have pain, follow your doctor's instructions to relieve it. Pain from cancer can almost always be controlled. Use pain medicine when you first notice pain, before it becomes severe.
- Eat healthy food. If you do not feel like eating, try to eat food that has protein and extra calories to keep up your strength and prevent weight loss.
- Get some physical activity every day, but do not get too tired.
- Get enough sleep, and take time to do things you enjoy. This can help reduce stress.
- Think about joining a support group. Or discuss your concerns with your doctor or a counselor.
- If you are vomiting or have diarrhea:
- Drink plenty of fluids to prevent dehydration. Choose water and other clear liquids. If you have kidney, heart, or liver disease and have to limit fluids, talk with your doctor before you increase the amount of fluids you drink.
- When you are able to eat, try clear soups, mild foods, and liquids until all symptoms are gone for 12 to 48 hours. Other good choices include dry toast, crackers, cooked cereal, and gelatin dessert, such as Jell-O.
- Do not smoke. Smoking can slow healing. If you need help quitting, talk to your doctor about stop-smoking programs and medicines. These can increase your chances of quitting for good.
- If you have not already done so, prepare a list of advance directives. Advance directives are instructions to your doctor and family members about what kind of care you want if you become unable to speak or express yourself.
Protect your skin
- Always wear sunscreen on exposed skin. Make sure to use a broad-spectrum sunscreen that has a sun protection factor (SPF) of 30 or higher. Use it every day, even when it is cloudy. While you are outdoors, apply more sunscreen every 2 to 3 hours or anytime your skin gets wet.
- Wear a wide-brimmed hat, a long-sleeved shirt, and pants if you are going to be outdoors for very long.
- Stay out of the sun during the midday hours (10 a.m. to 4 p.m.), when UV rays are strongest.
- Avoid sunlamps and tanning salons.
Learn more
- Cancer: Controlling Cancer Pain
- Cancer: Controlling Nausea and Vomiting From Chemotherapy
- Cancer: Home Treatment for Constipation
- Cancer: Home Treatment for Diarrhea
- Cancer: Home Treatment for Fatigue
- Cancer: Home Treatment for Mouth Sores
- Cancer: Home Treatment for Pain
- Cancer: Home Treatment for Sleep Problems
- Cancer Support: Managing Stress
- Eating Well During Cancer Treatment
- Hair Loss From Cancer Treatment
- Quitting Smoking
- Skin Cancer: Preventing It and Watching for Early Signs
Watch
Complementary Treatments
Some people use complementary therapies along with medical treatment. They may help relieve the symptoms and stress of cancer or the side effects of cancer treatment. Therapies that may be helpful include:
- Acupuncture to relieve pain and other symptoms.
- Meditation or yoga to relieve stress.
- Massage and biofeedback to reduce pain and tension.
- Breathing exercises to help you relax.
Talk with your doctor about any of these options you would like to try. And let your doctor know if you are already using any complementary therapies. They are not meant to take the place of standard medical treatment. But they may help you feel better and cope better with treatment.
Learn more
Watch
Getting Support
Relationships take on new importance when you're faced with cancer. Your family and friends can help support you. You may also want to look beyond those who are close to you.
- Reach out to your family and friends.
Remember that the people around you want to support you, and asking for help isn't a sign of weakness.
- Tell them how they can help.
Your friends and family want to help, but some of them may not know what to do. It may help to make a list. For example, you might ask them to:
- Run errands or pick up kids.
- Deliver meals or groceries to your home.
- Drive you to appointments.
- Go to doctor visits with you and take notes.
- Look for help from other sources.
Places to turn for support include:
- Counseling.
- Counseling can help you cope with cancer and the effect cancer is having on your life. Different types of counseling include family therapy, couples therapy, group counseling, and individual counseling.
- Your health care team.
- Your team should be supportive. Be open and honest about your fears and concerns. Your doctor can help you get the right medical treatments, including counseling.
- Spiritual or religious groups.
- These groups can provide comfort and may be able to help you find counseling or other social support services.
- Social groups.
- Social groups can help you meet new people and get involved in activities you enjoy. Focus on activities that bring you comfort, such as spending time outdoors or being with children.
- A cancer support group.
- Cancer support groups offer support and practical advice. You can hear others talk about:
- What it's like to live with cancer.
- Practical ways to manage your cancer treatment and its side effects.
- Ways to cope with your illness.
Learn more
Watch
Credits
Current as of: October 25, 2023
Author: Healthwise Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: October 25, 2023
Author: Healthwise Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
 Skin self-examination
Skin self-examination Melanoma skin cancer sign: Asymmetry
Melanoma skin cancer sign: Asymmetry Melanoma skin cancer sign: Border that is irregular
Melanoma skin cancer sign: Border that is irregular Melanoma skin cancer sign: Color variation
Melanoma skin cancer sign: Color variation Melanoma skin cancer sign: Diameter
Melanoma skin cancer sign: Diameter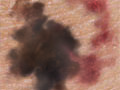 Melanoma skin cancer sign: Evolution
Melanoma skin cancer sign: Evolution Melanoma
Melanoma Caring for Your Implanted Port
Caring for Your Implanted Port Protecting Your Skin From the Sun
Protecting Your Skin From the Sun Skin Cancer Prevention: How to Check Your Skin
Skin Cancer Prevention: How to Check Your Skin
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.