Pressure Injuries: Prevention and Treatment
Overview
How can pressure injuries be prevented?
Relieving and spreading out pressure is the most important part of both preventing and treating pressure injuries. Putting pressure on one spot for long periods of time damages the skin and underlying tissues. Pressure can be relieved and spread in several ways. Often a combination of these is best.
- Change position often.
- In a bed, change position every 2 hours. Learn how to move yourself so that you avoid folding and twisting your skin.
- In a wheelchair or other type of chair, shift your weight every 15 minutes.
- Try not to slide or slump across sheets in a chair or bed. Recliner chairs are likely to allow slipping, so don't sleep in a recliner. Try to keep the head of a bed, a recliner chair, or a reclining wheelchair raised no more than 30 degrees.
- Take good care of your skin.
- Bathe as often as needed to be clean and comfortable. Use gentle soap, and use warm (not hot) water. Be careful not to scrub the skin too hard.
- If you have problems with bowel or bladder control, clean your skin right away if it gets soiled or wet. Use a protective barrier cream, lotion, or ointment to protect your skin from wetness. Use pads or briefs that absorb moisture and pull it away from your skin.
- If you have dry skin, use moisturizing cream or lotion to keep your skin from drying out and cracking.
- Check your skin every day for signs of pressure injuries. Pay special attention to bony areas such as the hips, elbows, knees, and heels. Also watch for pressure from sources such as:
- Body parts or skin folds, especially if you're overweight.
- Chair arms, parts of wheelchairs, braces, or other places where you rest your elbows or other body parts.
- Medical equipment such as oxygen masks or oxygen tubing.
- Make healthy choices.
- Eat healthy foods with enough protein, and get plenty of fluids. That can help damaged skin heal and help new skin grow.
- Stay at a healthy weight. Both weight gain and weight loss can make pressure injuries more likely. Weight changes can also cause problems with support equipment that no longer fits.
- Don't smoke. Smoking dries the skin and reduces blood supply to the skin.
- Talk to your doctor about pressure-relieving cushions and pads.
- Use special support surfaces. There are mattresses, bed covers, and chair cushions designed to help reduce and spread pressure.
- Ask your doctor which cushions and pads might help you. Some products, such as doughnut-type devices, may actually cause pressure injuries or make them worse.
If you or someone you care for is not able to move much, it's important to prevent pressure injuries and to check the skin every day. If you think that a pressure injury is forming, take steps to treat it. Talk to your doctor or nurse about what more you can do.
What can you do to treat a pressure injury?
If a pressure injury forms, use prevention steps to relieve pressure and protect the skin. It's also important to keep the sore clean, covered, and slightly moist. Used together, these steps can help keep the sore from getting worse and help your skin heal.
- Keep the sore clean.
Clean the pressure injury every time the bandage (dressing) is changed. Saline is often used for cleaning. This is a saltwater solution that you can buy at a drugstore. But there are many cleansing products for wounds. Your doctor will recommend a cleansing solution for you. In some cases, it may be okay to use tap water to clean the wound.
- Do not use cleansers made for healthy skin on an open wound.
- Avoid antiseptic solutions such as Betadine, Hibiclens, and hydrogen peroxide. These can damage new and normal tissue.
- Do not wash an open wound with water from a well. Most tap water is safe, but follow the advice of your doctor or nurse.
- Keep the sore covered and slightly moist.
Your doctor will recommend a bandage for the pressure injury. There are many types of bandages. Over time, your doctor may have you use several different kinds of bandage as the pressure injury heals.
The general idea is to keep the wound a little moist and not let it dry out between bandage changes.
- Keep the moist part of the bandage right down in the sore, placed loosely against the healing tissue.
- Cover the moist bandage with a dry bandage to help keep the sore clean and to keep the healthy skin around the pressure injury dry.
- Treat pain as needed.
Pain may or may not be a problem with pressure injuries. Some people who have pressure injuries don't need any pain medicine. Some need it just when the sore is being treated. And some need it on a regular schedule. If you have pain, talk to your doctor.
What other treatments may be used to treat pressure injuries?
Treatment focuses on preventing a pressure injury from getting worse and on making the skin healthy again. It may include:
- Taking pressure off the area, changing positions often, and spreading body weight evenly with special mattresses, pads, or other support.
- Keeping the wound clean and covered with a bandage. The doctor will tell you how to care for your wound. You may need to keep the wound a little moist and not let it dry out between bandage changes.
- Eating a healthy diet with enough protein.
- Having debridement. This is when the doctor removes dead tissue from the wound to promote healing.
- Having surgery. Severe pressure injuries may be treated with surgery. A tissue flap or skin graft may be needed.
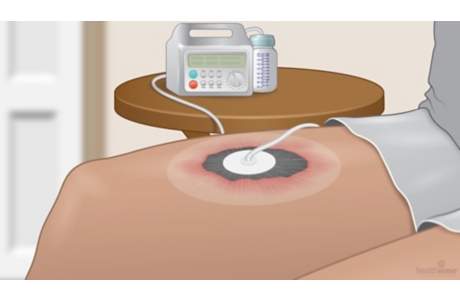
Negative-pressure wound therapy, also called vacuum-assisted closure, may be used to help with healing.
Researchers continue to study these and other treatments for wounds, including electrical stimulation, hyperbaric oxygen therapy, platelet-derived growth factor, and ultrasound therapy.
How can you tell if a pressure injury is healing as it should?
As you treat a pressure injury, you will know that it's healing correctly if:
- The sore is getting smaller.
- Pinkish tissue is forming along the edges of the sore, gradually moving toward the center.
- The sore bleeds a little. This means that there's blood circulation in the area, which helps healing.
After a pressure injury is healed, the skin is still very fragile. It's easy for the skin to break down again, especially in the first month after the sore is healed. To decrease the risk that the pressure injury will come back, slowly return to the positions that put pressure on the area where the sore was. For example, apply pressure for no more than 15 to 30 minutes at first. Then check to see if the redness fades within 15 minutes after you take the pressure off. Talk to your doctor or nurse about a plan for returning to your normal positions and activities after a pressure injury is healed.
How do you know if a pressure injury is infected?
Open wounds, such as pressure injuries, are easy places for infections to start. Your doctor will watch for signs of infection, and you can help. Tell your doctor if you notice:
- Redness or warmth in the skin around the sore, or red streaks leading away from the sore area.
- Tenderness around the sore.
- Pus in the drainage from the sore.
- A bad smell from the sore or from the bandage.
- Fever.
To treat an infection, you may use medicine, such as antibiotics, along with special care of the wound. You and the people around you will also be taught to take steps to keep germs from spreading to other parts of your body or to other people. These steps include keeping the sore covered at all times except during treatment, good hand-washing before and after caring for the pressure injury, and properly wrapping and throwing away used bandages.
How well do pressure injuries heal?
How well a pressure injury heals depends in part on its stage.
- Most stage 1 and stage 2 pressure injuries will heal within several weeks with proper treatment. Early treatment can help prevent damage and keep a sore from progressing to a more serious stage.
- Stage 3 and 4 pressure injuries are harder to treat. They can take months or even years to heal. Continued care and treatment can prevent complications such as infection, more tissue damage, and pain.
Credits
Current as of: November 16, 2023
Author: Healthwise Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: November 16, 2023
Author: Healthwise Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.